How To Start A Support Group

It is vital for people living with Parkinson's disease (PD) and care partners to make social connections and find support. Whether you have been newly diagnosed with PD, have been living with PD for a while, or are caring for someone with PD, connecting with others can help.
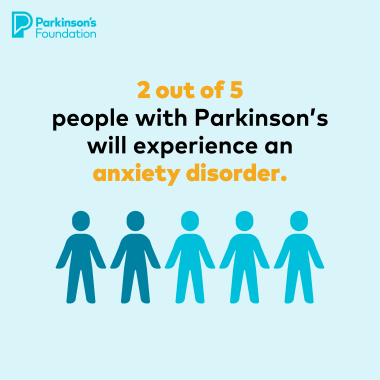
Challenges associated with PD, including movement symptoms, cognitive changes and emotional fluctuations, can lead to social withdrawal and isolation. Engaging in social activities can provide a valuable support network, combat feelings of depression and loneliness, maintain cognitive function and emotional well-being.
Why are support groups important?
Finding the right support group can help you build your PD community. In these groups, people share their experiences, learn from each other, and get access to resources that suit their needs.
Through these connections, individuals affected by PD not only find companionship and empathy but also gain a sense of belonging and resilience that can improve their PD journey. With the support provided by groups, people affected by PD can navigate the condition with greater confidence, hope and well-being.
Types of Support Groups
There are many kinds of PD support groups available. They include:
-
People with PD: These groups focus on people living with PD, allowing them to share their experiences, learn from each other and offer support.
-
Care partners: Care partners know Parkinson’s and its ups and downs. These groups provide a space for care partners to share their challenges, receive support and learn coping strategies.
-
Combined Groups: Many support groups welcome people with PD and care partners, fostering a supportive environment where both groups can share experiences, offer mutual support and learn from each other's perspectives.
-
Young-Onset PD (YOPD): These groups cater to those diagnosed with PD at a younger age, addressing unique challenges and concerns relevant to them.
-
Virtual: Online communities that allow members to share experiences from the comfort of their own home.
-
In-person: Face-to-face gatherings where people can meet to discuss their experiences.
Tips for Starting A Support Group
If you have not found a support group that is the right fit for you, consider starting your own. Explore our Support Group Guide for a step-by-step planning process. The most important part of any support group is to ensure members feel accepted, respected and comfortable when attending the group.
Building and launching a support group requires planning, organization and attention to detail. The “let’s get started” phase can be overwhelming, but breaking down a big task into smaller tasks can make planning more manageable. Consider these key aspects before launching a support group:
-
Who will attend this group?
This step is crucial for building the foundation of your support group. Make sure you know your audience before you figure out any specific details about the group. You can choose from the types of support groups above to get started.
-
Where will the group take place?
If you decide to start an in-person support group, start looking for a potential meeting space. The location can make or break your group. Rule out locations that are not easily accessible.
These locations are generally open to hosting support groups:
-
Public libraries
-
Hospitals
-
Community living centers
-
Places of worship (remember accessibility requirements for older buildings)
-
Town halls
-
Senior centers
-
Senior living facilities or nursing homes
Each community is unique, so consider what other possibilities could exist in yours. Talk to people and let them know what you are looking for. Let others spread the word to help you secure a solid, consistent location.
-
How often will your group meet?
Many PD support groups meet monthly. Find the frequency that works for your group. Consider that the more often you meet, the faster members can become fatigued, and more planning will be required. Meeting less than once a month can limit the group’s ability to build relationships.
Having a consistent day of the month (for instance, the second Tuesday of each month) helps people to remember when the group meets.
An even bigger consideration is time of day — will you meet in the morning, afternoon, or evening? Make the decision that works best for you as a leader and ask potential participants for feedback. Establishing a regular time and place will help your group expand as more people become aware of its existence.
-
What is the support group’s format?
There are many formats you may choose to use for your group. The best advice is to stay flexible. You may start out with a formal meeting agenda and decide that you want to change things up and go less formal. Listen to what your group members tell you!
To help “break the ice” at the start of each meeting, particularly for new members in attendance, introductions are a great technique. Not only does everyone get a chance to say something, but it also helps members remember names and relationships.
-
How long are meetings?
Support groups usually meet for no more than 90 minutes. It also may be helpful to design a break halfway through for refreshments and a rest room break. Find what works best for the group.
Parkinson’s Education and Finding Guest Speakers
Besides planning the basics, it is also important to consider things like topics for each meeting and if you plan to have a guest speaker. One common need for the Parkinson’s community is disease education.
Guest speakers can include:
-
Local PD experts you or group members know.
-
Staff from a Parkinson’s Foundation Centers of Excellence
-
Parkinson’s Foundation volunteer. Email us at Volunteer@Parkinson.org and we can help connect you to someone in your area.
If you are not sure where to start, ask your group members for suggestions and topic recommendations.
Promoting Your Group
Promotion is essential for a successful support group. Word of mouth can help but it is typically not enough. Consider creating a flyer or letter announcing the group, starting date, location and contact person. If you have a speaker scheduled, be sure to include that information and the topic they will be discussing.
Social media can also be helpful in raising awareness of your new group. It can be especially helpful for reaching younger people with PD and their care partners. Managing a social media page could be a great volunteer role for a group member to take on.
How To Find A Support Group
Here are two ways to find a local PD support group:
-
Visit our Parkinson’s Foundation Chapter page to search for one in your area.
-
Call our Helpline at 1-800-4PD-INFO (1-800-473-4636) or email Helpline@Parkinson.org.
For more information on starting a support group, check out our Support Group Guide.
Related Materials
Pain in Parkinson's Disease
Occupational Therapy and PD
Nutrition and PD
Related Blog Posts


Shaping the Future of Parkinson’s Policy: Meet Our Chief Strategy and Policy Officer