Explorando las terapias complementarias y la medicina funcional en el cuidado del Parkinson

La medicina integrativa combina la medicina basada en la evidencia con terapias complementarias de eficacia comprobada y la medicina funcional; tratamiento que pretende atender a la persona en su totalidad, para controlar los síntomas de la enfermedad de Parkinson (EP). Explore cómo los tratamientos no farmacológicos, como los masajes, la acupuntura, la terapia con luz roja y el CBD, se utilizan a veces para favorecer el bienestar junto con los cuidados tradicionales del Parkinson.
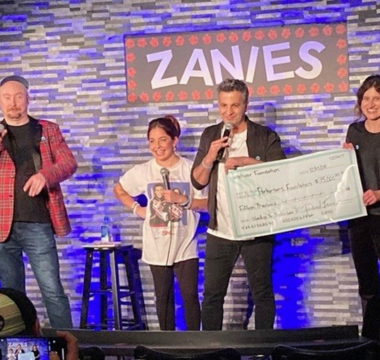
El siguiente artículo se basa en una de las Charlas con Expertos - Expert Briefings de la Parkinson's Foundation, que explora las terapias complementarias y la medicina holística en el cuidado del Parkinson, presentada por la Dra. Britt Stone, profesora clínica adjunta, división de Trastornos del Movimiento, Departamento de Neurología en el Vanderbilt University Medical Center (VUMC, por sus siglas en inglés), un Centro de Excelencia de la Parkinson's Foundation y directora de operaciones clínicas para las clínicas de neurología del campus principal de VUMC.
Un puente entre la medicina moderna y los cuidados complementarios
Las terapias tradicionales de medicina occidental incluyen los cuidados que pueda recetar su neurólogo, ya sea levodopa u otros medicamentos recetados, fisioterapia o terapia ocupacional o psiquiatría o la recomendación de un asistente de salud a domicilio.
La medicina integrativa combina la medicina con terapias complementarias de eficacia probada para fomentar un bienestar óptimo.
-
La medicina funcional se engloba dentro de la medicina integrativa; busca identificar la causa raíz de la enfermedad y tratar a la persona en su totalidad mediante un plan de atención personalizado.
-
Las terapias complementarias son un elemento de la medicina funcional: pueden incluir atención plena (mindfulness), terapia artística o de danza u otros tratamientos.
Una mirada más profunda a la medicina funcional
Vivir bien con Parkinson requiere un manejo continuo: los medicamentos adecuados, ejercicio estructurado, una dieta equilibrada y la capacidad de adaptarse a las necesidades cambiantes. La medicina funcional también adopta un enfoque integral de la atención, haciendo hincapié en factores constantes de nutrición, salud intestinal y estilo de vida.
En esencia, la medicina funcional incorpora a la vida diaria hábitos, rutinas y ritmos que contribuyen a la salud general. A partir de ahí, las terapias específicas para atender las necesidades individuales se integran en un plan de cuidados. Éstos pueden incluir ejercicios adaptados, suplementos, hierbas medicinales u otras terapias complementarias.
La medicina funcional también puede incluir pruebas de laboratorio o diagnósticas para descubrir si factores como la genética o la exposición ambiental, incluidos los alérgenos, influyen en el funcionamiento del organismo. Las pruebas de laboratorio, que no siempre cubre el seguro, podrían incluir la detección de moho ambiental u otras toxinas en el organismo o evaluaciones de:
-
Niveles de vitaminas y minerales
-
Salud intestinal
-
Marcadores inflamatorios
-
Sensibilidad alimentaria
Hasta cierto punto, la genética, el medio ambiente, las enfermedades previas y los factores sociales y de conducta influyen en los resultados de la salud de cada persona. La medicina funcional toma en cuenta todos estos aspectos y busca ralentizar la progresión de la enfermedad y optimizar la calidad de vida.
Terapias complementarias
El Parkinson puede causar diversos síntomas no motores, como rigidez, dolor, ansiedad, sueño y cambios de humor, y es posible que los medicamentos no los alivien todos. Las terapias complementarias no farmacológicas se han ido generalizando para el tratamiento de los síntomas del Parkinson, sobre todo para aquellos que no responden tan bien a los medicamentos recetados.
Ciertas terapias complementarias que fomentan las conexiones sociales y la creatividad al tiempo que promueven el propósito y el juego han demostrado mejorar la calidad de vida. Un metaanálisis de 2020 demostró que el baile mejoraba los síntomas motores y no motores y la calidad de vida en personas con Parkinson. Un programa de seis semanas de arteterapia con barro para Parkinson mostró una disminución de la depresión, el estrés y el pensamiento obsesivo-compulsivo entre los participantes.
Algunas terapias complementarias están basadas en la filosofía y la medicina chinas y en el concepto de chi o qi, la energía o fuerza vital que anima a una persona. Se cree que un chi lento o deficiente provoca enfermedades. El trabajo de respiración mente-cuerpo, como el Tai Chi y el qigong, utilizados para mejorar el equilibrio, el funcionamiento y el estado de ánimo en el Parkinson, busca mejorar el flujo de energía.
Hay otras terapias como:
Acupuntura: Un estudio demostró que la acupuntura, que también busca equilibrar el flujo de energía, podría aliviar el dolor musculoesquelético en el Parkinson. Otros informes de casos y estudios clínicos muestran que la acupuntura puede mejorar las actividades de la vida diaria de las personas con Parkinson. La punción seca, una técnica de fisioterapia utilizada para aliviar el dolor, acelerar la curación y mejorar el movimiento, también utiliza pequeñas agujas finas, pero la técnica es diferente y el objetivo es el tratamiento del músculo específico, en lugar de mejorar el flujo de energía.
Masaje: Se utiliza para aumentar la relajación y aliviar los espasmos y calambres musculares. Una revisión de 2020 que analizaba 12 estudios acerca de la terapia de masaje y sus beneficios en el Parkinson descubrió que:
-
Múltiples tipos de masaje inducían relajación.
-
Los participantes reportaron mejoras en el estado de ánimo, la fatiga, el sueño y el dolor.
-
Algunas investigaciones demuestran que los tipos de masaje neuromuscular, como el shiatsu, el tui na y el masaje neuromuscular tailandés, podrían mejorar los síntomas motores.
Terapia de luz roja: Las nuevas investigaciones muestran que la terapia con luz roja de bajo nivel, también llamada fotobiomodulación, puede tener un potencial neuroprotector en el Parkinson. Sin embargo, se necesitan más estudios. Los beneficios potenciales para la salud de la terapia con luz roja fueron descubiertos por científicos de la NASA que, al experimentar con diodos emisores de luz para estimular el crecimiento de las plantas, observaron que las luces también aceleraban la cicatrización de las heridas.
La terapia con luz roja se utiliza actualmente como parte de la terapia fotodinámica en dermatología para tratar ciertos tipos de cáncer de piel (la luz roja activa un fármaco fotosensibilizante). También se utiliza para tratar la psoriasis y el acné. Se cree que la terapia con luz roja actúa estimulando las mitocondrias de las células tratadas, lo que conduce a una actividad celular más eficaz y al crecimiento de nuevas células. Es importante proteger los ojos cuando se utiliza cualquier tipo de terapia con luz roja.
Cannabidiol (CBD): Este compuesto se encuentra en las plantas de cannabis como cáñamo y marihuana e interactúa con el sistema endocannabinoide del organismo. Los receptores CB1 y CB2, componentes clave de este sistema, intervienen en la comunicación entre las células cerebrales y la salud intestinal e inmunitaria.
En la marihuana, hay mayores concentraciones de THC, el compuesto que produce un efecto psicoactivo. El cáñamo suele ser rico en CBD, un compuesto que puede ser útil para el sueño, la ansiedad o el dolor, aunque se necesita más investigación. Epidiolex es una forma recetada de CBD, aprobada por la Food and Drug Administration (Administración de Alimentos y Medicamentos) para tratar ciertos tipos de convulsiones.
La legalización de la marihuana medicinal y recreativa varía según el estado. Puede haber consideraciones de seguridad, dependiendo de sus síntomas o de los medicamentos que esté tomando.
Incorporación de la terapia complementaria a su rutina
La creación de un plan personalizado y equilibrado para manejar el Parkinson puede ayudarle a mantener su independencia. Las terapias complementarias, el contacto terapéutico, un profesional que escuche, el tiempo de descanso y la atención plena pueden mejorar la calidad de vida y la sensación de bienestar.
A la hora de decidir qué terapias podrían beneficiarle, piense en sus objetivos y en los síntomas que más le molestan. Mantenga una conversación abierta con su equipo de atención médica y analice las opciones de tratamiento disponibles. Hablar acerca de las posibles terapias con su doctor puede ayudarle a evitar posibles interacciones y garantizar los mejores resultados. Conectarse en línea o en persona con personas de la comunidad de Parkinson también puede darle la oportunidad de hablar acerca de lo que ha funcionado para otros y compartir sus propias experiencias.
Considere terapias que se ajusten a sus necesidades y que además sean accesibles, asequibles y manejables. Añada un elemento nuevo, observe los efectos o beneficios y ajuste o cambie los planes, con la opinión de su equipo de atención médica, según sea necesario.
Aprenda más
Explore nuestros recursos acerca de las terapias complementarias y el manejo de los síntomas en el Parkinson: