10 Tips for Playing Pickleball to Stay Active with Parkinson’s
🧠 What will you learn in this article?
This article highlights tips for playing Pickleball to stay active with Parkinson’s disease. It discusses:
- When it comes to Parkinson’s symptoms, Pickleball is an aerobic workout that strengthens balance, agility, builds muscle and cognitive function.
- The importance of exercise for people with Parkinson’s.
- 10 ways people with Parkinson’s can stay safe while playing pickleball.

For many people with Parkinson’s disease (PD), pickleball has become a new way to infuse exercise with socialization.
Exercise is a vital part of Parkinson’s disease management. It helps maintain balance, mobility, flexibility and overall quality of life. Research shows that consistent exercise — at least 2.5 hours per week — can slow symptom progression and improve physical and emotional wellbeing.
Pickleball is a paddle sport played indoors or outdoors on a court smaller than a traditional tennis court. It is played in singles or doubles with a light, plastic ball. USA Pickleball sets official rules and supports programs nationwide. One reason the sport is popular is because it is easy to learn but challenging, and is accessible for people of all ages and abilities.
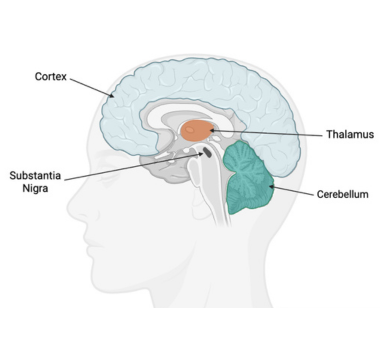
When it comes to Parkinson’s symptoms, Pickleball is an aerobic workout that strengthens balance, agility, builds muscle and cognitive function. A player’s ability to think and respond quickly while playing pickleball can boost brain activity. Additionally, it is a great way to socialize, an important part of living well with Parkinson’s as isolation following a diagnosis can lead to depression, a common PD symptom.
Trying a sport like pickleball can make staying active feel social and motivating. Setting a small, achievable goal, such as playing pickleball once a week, can help turn exercise into a habit you look forward to rather than a chore.
Here are 10 tips for playing Pickleball to stay active with Parkinson’s:
- Get clearance from your neurologist.
Before starting any new exercise, talk to your neurologist or PD doctor to make sure starting a new sport or exercise is safe. They may recommend seeing a physical therapist to prevent injuries. - Work with a physical therapist (PT).
Telling your physical therapist that you are playing pickleball or plan to start can help them customize your sessions to improve movement and mobility. PT can address stiffness and help you train to keep on-court movements safe. PT can also help build strength and improve coordination. - Incorporate other exercises to up your pickleball game.
Pickleball is a great way to evolve your exercise routine. Explore other exercises, like PD Health @ Home on-demand videos that address PD-specific balance, agility and movements between games. - Warm up before playing pickleball to prevent injury.
Before playing, develop a pickleball warm-up routine that works for you. This is a great opportunity for your physical therapist to weigh in.
Building PD Awareness on the Court
The Parkinson’s Foundation has partnered with Selkirk to raise awareness of the benefits of exercise for people living with Parkinson’s. For every pickleball paddle sold, Selkirk will donate 12% of sales to the Parkinson’s Foundation, a percentage that represents the 1.2 million people projected to be living with Parkinson’s by 2030.
- Don’t play hurt.
Rest when your body needs more recovery time. Parkinson’s symptoms can change from day to day, listen to your body and don’t push yourself on days you need more rest. - Play during “on” times, when symptoms are most manageable.
Medications like levodopa, commonly used for PD, help manage symptoms. As PD progresses, the brain's response to these medications may change, which can lead to symptom fluctuations, known as "on" and "off" periods. If possible, schedule pickleball games during "on" periods, when medication is working well. - Use pickleball to build community and bond with a family member or spouse.
Playing doubles can also help reduce court coverage and build relationships. Joining a pickleball league could be a great opportunity to start a new pastime with your adult child or spouse. - Always stay hydrated.
On or off the court, being dehydrated can make some PD symptoms worse, including constipation, swallowing issues and low blood pressure. On the court, not drinking enough liquids can bring muscle cramps and dizziness. Hydrate whenever possible. - Modify the game as needed.
Adjust game lengths, build in more breaks or stick to playing doubles. Joining a PD league or playing with others who have Parkinson’s is a great way to build in modifications. - Explore Pickleball for Parkinson’s events.
Join an upcoming Pickleball for Parkinson’s event or start your own. For qualifying events, the pickleball paddle manufacturer Selkirk offers a sponsorship. Learn more.
Pickleball can be more than a game. For people living with Parkinson’s, it can be a powerful tool for movement and connection —essential elements of living well with PD.
Exercise Resources
The best way to see benefits is to exercise consistently. People with PD enrolled in exercise programs for longer than six months, regardless of exercise intensity, see significant gains in functional balance and mobility compared to shorter programs. Explore our exercise resources:
-
Find a PD exercise class near you through our Parkinsons’ Foundation Chapters or contact our Helpline at 1-800-4PD-INFO (1-800-473-4636) or Helpline@parkinson.org.
-
Explore Fitness Friday on-demand exercise classes through our PD Health @ Home program.
-
Celebrate movement with your local PD community. Sign up for a Moving Day event.
Explore tips and learn more about exercise and Parkinson’s research on our Parkinson’s and exercise page.
Related Materials
Related Blog Posts

10 Tips for Playing Pickleball to Stay Active with Parkinson’s