My PD Story

Ann Boylan
I’d like my Parkinson’s story to not be about living with limitations but rather about living with possibility.
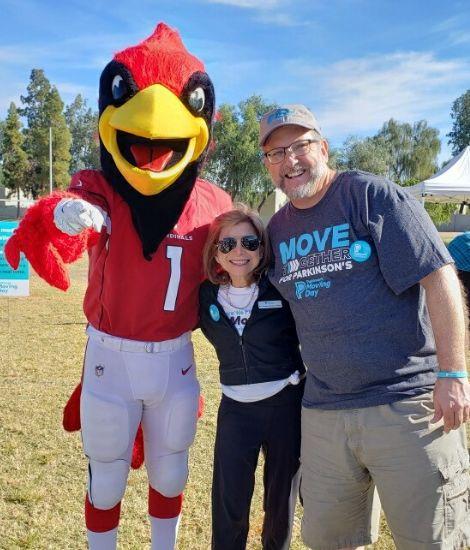
In 2015, my hometown of Union City, CA, and my fellow Mark Green Community Sports Center class attendees became the first Moving Day team, and received a Parkinson's Foundation community grant that made Union City’s Mark Green Sports Center the first Parkinson’s exercise program in the South East Bay a reality! Robert Magbanua Jr, our Parkinson’s fitness leader, trainer and program designer, and Corina Hahn, community program administrator were instrumental in making this happen.
Over the years this program has grown to include caregiver support and classes that are offered five days a week and at home through Zoom. Robert’s charisma and enthusiasm keeps him in demand for speaking and leading attendees at Parkinson’s Foundation events all around the San Francisco Bay Area.
About the same time as our first Moving Day event, I also became an advocate for awareness of the unique needs of women diagnosed with Parkinson's disease. In good part, looking at inequities when it comes to decisions about efficacy of drugs and treatments, that in the first place ignored gender differences in research with predominantly male subjects, and therefore skewed dosages and outcomes. Moreover single women, either without spouses or widowed, are more often relegated to nursing home care because they lack the means to advocate for aging in place, a familiar home, or for a clean home-like setting with the privacy and dignity of individual care.
These days my Parkinson’s story focuses on living with possibility thanks to a Parkinson’s breakthrough now dating back 20 years ago called deep brain stimulation (DBS) surgery, which I had two months ago. Still a miracle of science, it is a precision-driven, courageous team effort that has given me time in which some of the most debilitating features of Parkinson’s such as tremor and dystonia pain might be kept at bay, and I can have time to pursue activities and commitments that promote heart, hope, energy, awe, curiosity and love.
My Parkinson’s story? It is about “flourishing” with Parkinson’s disease and the “community to be found within it.”
Our Moving Day San Jose “Hop on the Union City A Train” team begins its ninth year raising funds, awareness and heartfelt support for the Parkinson’s Foundation. Let's not have to wait another 20 years for a breakthrough for Parkinson's!
Thanks to my family and especially, my friends, my "ohana," my family through love, My Parkinson’s story continues!
Sex and gender differences can drastically impact health and are important to consider when it comes to Parkinson's. Explore our Women & Parkinson's page.
Related Materials
More Stories
from the Parkinson's community