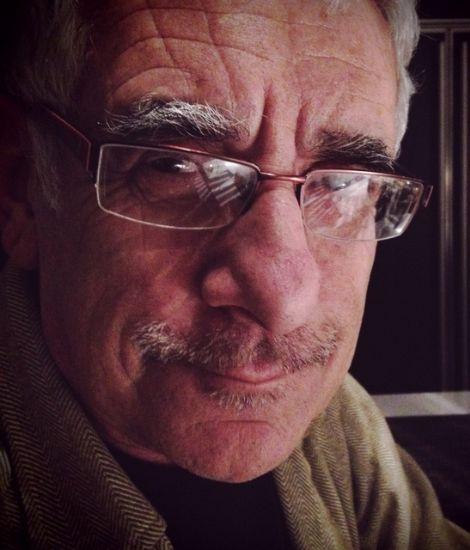
In 2015, while walking with my wife, Jody, in our neighborhood, I suddenly found myself bent over and taking tiny, rapid, repetitive steps. I knew I was moving too fast but could not stop myself. Jody thought I was kidding — until the moment I fell down on a neighbor's lawn.
A passing driver slowed down to ask if I was okay. I was alright, but thought the experience was odd.
I saw a neurologist friend a week later. In retrospect, I’m not sure how I knew that I needed to see a neurologist; perhaps, given my decades as a pediatrician, my clinical judgment was operating on a subliminal level.
My friend did several clinical tests — watching me walk, evaluating my facility with finger-to-nose movements, rapidly opening and closing my hands and so on. My history included loss of my sense of smell (I’ve never been able to discern the nuances of red wine) and horrible handwriting (not just because I'm a physician).
The neurologist said that I had a mild case of Parkinson's disease (PD), placed me on levodopa and suggested that I begin physical activities to stave off progression. Though I didn’t know much about Parkinson’s, I began doing a movement class, Pilates, a boxing balance-and-agility class, doubles tennis and nine holes of golf once a week. I looked at all of this as the upside of PD —getting to doing activities that I enjoy.
But I felt a bit skeptical of the diagnosis. My symptoms were so mild that I wondered if I really had Parkinson's. This thought cropped up with some regularity, but I resigned myself to taking levodopa.
My symptoms haven’t progressed much in the ensuing seven years, except for some problems with balance; I now walk with a cane. I have an occasional minor tremor of my right index finger. This tremor, which worsens with stress, makes it hard to lift a spoon to my mouth (worse with soup), clip my fingernails (necessitating a monthly mani-pedi) or text with my iPhone (now I use a stylus, or dictate messages into the phone).
The most interesting thing about PD has been its effect on my relationship with my wife.
Jody started out knowing as little about the disease as I did, but our responses differ: where my glass is half full, hers tends to be half empty.
My approach to medical travail is simple: I use denial as a coping mechanism. It may seem illogical, since I’m a physician, but I do not need to delve into the Internet to understand what is happening to me. I simply rely on my physician to tell me what I need to know. My tendency is to assume that, since I’m being proactive with exercise, my symptoms will not progress.
As part of my routine, I participate in online movement programs geared to people with PD, who sign on from locations across the country. During these meetings, Jody and I see people whose symptoms are much worse than mine: persistent tremors, dystonia, masked face and uncontrolled movements.
I am unable to imagine myself with those symptoms, feeling convinced that my exercise regimen will ward them off. But interestingly, Jody goes to a dark place. She has said things like, "If you fall, I will not be able to lift you up. If things get worse, we will have to consider an assisted living arrangement.”
Jody has been helping and supporting me for thirty years, and now that I have PD, that need has intensified. Her efforts to make sure I’m taking care of myself include questions such as, "Are you wearing a belt?" and "Did you take a shower today?"
I react with silence. In my mind, silence means yes, but to Jody, it can seem passive-aggressive. It is true that I find these kinds of questions demeaning. Of course I am doing these things, and the fact that she feels compelled to ask me seems like a sign of either anxiety or a wish to make sure that I’m doing what I need to. My nonresponse is perhaps my way of trying to retain control over my life and my PD.
Sometimes Jody offers to do something for me, like taking my arm when we’re walking downstairs. I know I can maneuver them myself, but if I say so, and take my arm away, it can create tension between us. I find it difficult to explain that I understand her concerns, but that I also need to maintain a sense of control over my illness.
Jody and I are each trying make peace with our changed reality. Still, there is hope.
Resources available through the Parkinson’s Foundation help me handle my PD. I attend their online webinars to learn more about Parkinson’s and I exercise daily to manage my symptoms.
Attend a PD Health @ Home event to learn more about Parkinson’s and how to manage your PD symptoms.