Care Partner Deep Dive: Three Experts Discuss Sleep, Cognition and Mood in Parkinson's

How can care partners help their loved one with Parkinson’s disease (PD) manage the interplay between the Parkinson’s symptoms of sleep, cognition and mood?
Parkinson’s experts Aleksandar Videnovic, MD, Joseph F. Quinn, MD, and Martha Anne Tudor, MEd, NCC, LAPC, highlight these symptoms and ways care partners can help manage them. For a deeper dive on each topic, register for Parkinson’s Foundation Care Partner Program: Building a Care Partnership, a series of self-paced online courses designed with care partners in mind featuring PD experts.
How does exercise impact sleep, cognition and mood?
It is widely known that exercise is important in managing Parkinson’s symptoms, but how does it help?
- Cognition: Exercise is the single most valuable intervention for promoting cognition. Aerobic exercise has been indicated to enhance protective functions in brain tissue.
- Sleep: With the help of regular exercise our bodies will be more receptive to quality sleep at night.
- Mood: Having a regular exercise regimen can also help combat the depression and anxiety that can be associated with Parkinson’s.
→ Learn more about caring for a loved one experiencing mood changes with the Mood for the Person with Parkinson’s Disease care partner program.
What Parkinson’s medications could impact decline in sleep, cognition or mood?
When there is an issue with sleep, cognition or mood, there are many areas that should be considered when finding a solution.
- Cognition: Cognitive changes (including hallucinations) can be brought on by certain PD medications. Discuss PD medications with a doctor if you or your loved one are experiencing cognitive changes.
- Sleep: Medications with alerting properties should be avoided in the afternoon or evening to increase sleep quality. Taking carbidopa/levodopa before bed to ensure less “off” time during the night can help. Talk to your doctor about taking an anti-depressant to help increase quality of sleep.
- Mood: Many PD medications have mood side effects that can be managed if discussed with your prescribing doctor.
Ultimately, talk to your doctor about any medication concerns you may have.
→ Take our care partner program Cognitive Changes on a Continuum to learn more about caring for a loved one experiencing cognition changes.
How does a lack of sleep over time impact cognition and mood?
Sleep is vital for the body and mind.
- Cognition: Without good, consolidated sleep our ability to store and make memories is impacted, as is our ability to perform mental tasks.
- Mood: When we do not get enough sleep, we can experience symptoms that look like depression, but can also be a sign that our bodies are not functioning their best. Once we get the person’s sleep back on track, we can find out what else we are dealing with.
- Sleep: During sleep, our bodies “clean up” our pathways. Without good sleep, our body is not properly getting rid of toxins and waste.
→ Hear from a Parkinson’s expert and two care partners highlight The Role of Sleep in this care partner program.
How can cognitive changes and lack of sleep impact driving for a person with PD?
Driving is an important discussion to have before a person with Parkinson’s is no longer able to drive.
- Cognition: Allied health professionals, such as occupational therapists, are trained to monitor the ability to perform cognitively complex tasks such as driving.
- Mood: Driving schools are an objective accessor that can take the stress off the care partner to make the ultimate decision.
- Sleep: Sleep and fatigue are important considerations when deciding if a person with PD is safe to drive. Does the person with PD experience fatigue or need frequent naps? Do they fall asleep without warning?
Remember, it can be incredibly difficult to have driving privileges taken away. Approach this conversation with care and consideration. Consider speaking to a social worker or your support group for advice on the topic.
Which mood, cognition or sleep challenges tend to be the most challenging for care partners?
Care partners often experience Parkinson’s right along with their loved one and have a unique experience and viewpoint. You are not alone in your struggles!
- Cognition: Care partners can often experience frustration with the apathy or impulsivity that people with PD might experience.
- Mood: It is common for care partners to experience anger and frustration, specifically when witnessing the changes and limitations in their loved one’s day-to-day abilities. It can be helpful for care partners to try to “see it for the disease” rather than “just try harder.”
- Sleep: If the person with PD and the care partner shares a bed when the person with PD is not getting quality sleep, chances are that the bed partner isn’t either!
When it comes to mood, cognition or sleep challenges, always talk to your loved one’s doctor and care team about your questions and concerns. You can work together to find solutions that may improve with quality of life.
This article is based on the 2021 Care Partner Summit | Cumbre Para Cuidadores session Sleep, Cognition and Mood. Watch all sessions from the 2021 Care Partner Summit | Cumbre Para Cuidadores now.
Register for the Parkinson’s Foundation Care Partner Program: Building a Care Partnership to explore classes created for care partners.
Related Blog Posts

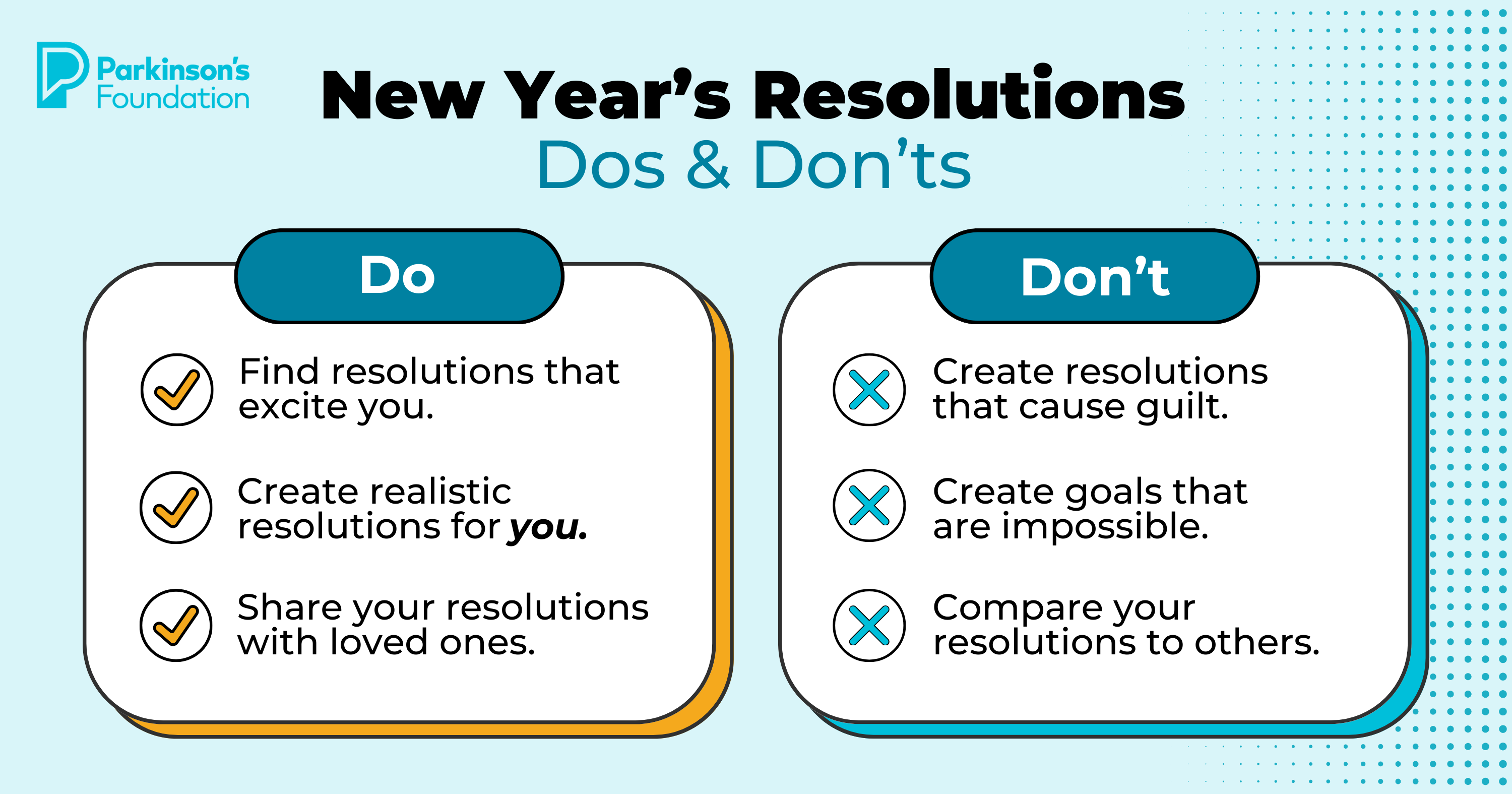
Start 2026 Strong: Simple Resolutions for Better Health

Celebrating 12 Milestones that Defined 2025