5 Volunteers Making a Difference
Across the country and beyond, Parkinson’s Foundation volunteers are going out and making a difference in the lives of people with Parkinson’s disease (PD) and their loved ones. They help us spread awareness and resources to those who need it most.

The dedication from our volunteers is what makes the Parkinson’s Foundation what it is today. We are honored to recognize five exceptional volunteers at the national level, who each received a 2024 volunteer award.

Dr. Reversa Joseph - Great Lakes Chapter
Paul Oreffice Volunteer of the Year
“Volunteering for the Parkinson's Foundation is more than just a commitment; it’s a deeply personal mission. Each effort, whether it’s a presentation, a lecture, or a podcast, is a step towards improving the lives of those affected by Parkinson’s, honoring my father’s struggle, and ensuring that every patient receives the comprehensive, integrative care they deserve.”

Esther Labib-Kiyarash – Southwest Chapter
Rising Star
“Along the way I have learned that there are many things, tips and tricks that the people who live the best with this disease share: exercise, positive thinking, being around others like themselves and giving back. The Parkinson’s Foundation is a great way to give back.”

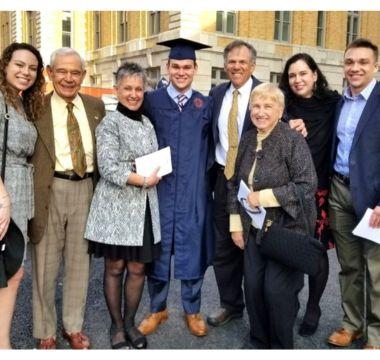
Roland and Shelley Frankel – Midwest Chapter
Top Fundraiser
As the somber saying goes, a parent should never have to bury their child. But in March 2023 Roland and Shelley Frankel had to do just that. Their son Graeme had been fighting Parkinson’s for five years and passed from an asthma-related emergency. To keep Graeme’s memory alive, the family decided to start a DIY fundraiser with the Parkinson’s Foundation.
Read Roland and Shelley’s full story

Debra Flynn – Florida Chapter
Community Service Award
“I really enjoy volunteering. I see it as another way to celebrate movement. I move my brain cells around; I motivate my soul to do good things; and volunteering moves forward the search for a cure.”
There are many powerful ways to get involved and support the Parkinson’s Foundation and our work to make life better for people with Parkinson's. Get started with our How You Can Help page. This page will give you options for volunteering, starting your own DIY Fundraiser, or even just donating to the cause.
You can also fill out a volunteer interest form to chat with our volunteer engagement team about how we can best put your skills to use. Help us bring life-saving information and resources to the hands of those who need them most.
Already a volunteer? Check out our course offerings today!
Related Materials
Related Blog Posts

Meet Volunteers Who are Making a Difference

From Passion to Action: 4 Volunteers Making a Difference