Parkinson's Medications 101

Medication plays a key role in managing Parkinson’s disease (PD), but it’s only one part of a broader care plan.
The following article is based on a Parkinson’s Foundation Expert Briefing exploring how medications fit into integrated, holistic Parkinson’s care, hosted by Danny Bega, MD, MSCI, associate professor of neurology, medical director and director of the Parkinson's Disease & Movement Disorders Center neurology residency program at Northwestern University Feinberg School of Medicine, a Parkinson's Foundation Center of Excellence. Dr. Bega is also the director of the Huntington's and Wilson’s diseases programs at Northwestern.
Understanding the Dopamine-Parkinson’s Connection
Parkinson’s is a progressive disorder linked to declining levels of dopamine, a brain chemical that influences movement, memory and many other vital body processes. Other brain chemicals, including norepinephrine and serotonin, can also be impacted in Parkinson's disease and influence symptoms.
As Parkinson’s advances, the number of brain cells making dopamine continues to decrease, and remaining cells struggle to store and release it. This leads to slowness of movement, tremor, rigidity and other motor symptoms. It can also cause various non-motor symptoms, such as constipation, loss of smell and thinking changes.
Managing Parkinson’s
Parkinson’s is a complex disease. There is no standard treatment. However, medications — along with exercise, comprehensive care, a nutritious diet and mindfulness practices — can manage Parkinson’s symptoms and help you live well.
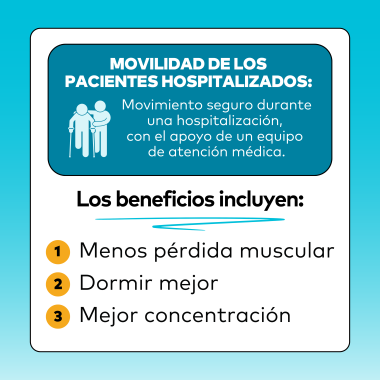
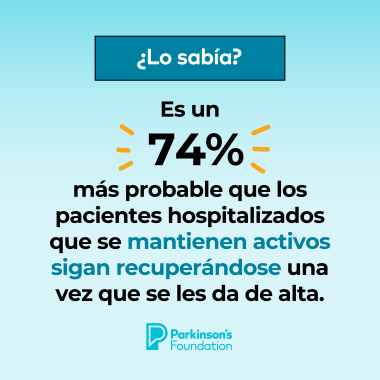
Establishing a regular exercise routine soon after diagnosis may help slow disease progression and can improve movement, strength, balance and mood. It can also help you sleep better. Staying social and engaged can reduce feelings of loneliness.
Your care team is equally important. Look for healthcare professionals with expertise in Parkinson’s, including a neurologist, speech-language pathologist, physical and occupational therapist, social worker and other healthcare professionals, to help manage your PD symptoms. Be sure to attend regular checkups.
The Role of Medication
Most Parkinson’s medications work to improve symptoms by either increasing dopamine in the brain or acting like dopamine. Levodopa is the most effective drug for managing Parkinson’s symptoms. During the course of Parkinson’s, most people will take levodopa at some point.
Anxiety and depression can also be common in Parkinson’s and can impact well-being even more than motor symptoms. Treating these symptoms using a combination of medication, such as an SSRI, SNRI or mirtazapine — a tricyclic antidepressant drug — along with therapy, stress management and staying active, can significantly decrease disability.
People newly diagnosed with Parkinson’s often wonder when to begin prescription medication. Studies show there is no benefit in holding off. Most doctors agree you should start medication when symptoms begin to bother you.
Because no two people experience PD in exactly the same way, treatments vary from person to person, as does the rate of progression. However, knowing the typical stages of Parkinson’s can help you anticipate changes:
-
In the first five years following diagnosis, you may find symptoms don’t significantly impact your daily life. Your doctor might recommend a clinical trial. Participation in Parkinson’s research can potentially give you early access to new treatments, improve care and lay the foundation for a cure.
-
Within one to 10 years, as symptoms begin to interfere with activities, most people with Parkinson’s can expect a long-lasting, steady response to medication.
-
Between five and 20 years after diagnosis, it becomes increasingly harder for the brain to store dopamine. Your body’s response to levodopa can become shorter and less efficient. This can lead to motor fluctuations — "on" periods, when medication works well, and "off" periods, when medication wears off and symptoms return. It is important to work closely with your doctor to adjust your treatment and find what works best for you.
-
After 10 or more years of living with Parkinson’s, a person can experience more significant issues. Some people can develop significant memory and thinking problems. Trouble with balance, falls and freezing, a temporary inability to move, can also become an issue. Your doctor can discuss medication adjustments or drug therapies or provide a referral to the right healthcare professional for your needs, which might include a neuropsychologist, psychiatrist, or a speech or occupational therapist.
Types of Medications Used in Parkinson’s
It can be common for people with Parkinson’s to take a variety of medications, at different doses and different times of day, to manage symptoms. This can include:
Dopamine agonists: Early on, drugs that stimulate dopamine in the brain, such as pramipexole, ropinirole and rotigotine, can usually treat Parkinson’s movement symptoms. Dopamine agonists pose less risk for dyskinesia — involuntary erratic movements that usually begin after a few years of levodopa treatment.
Side effects can include nausea, dizziness, sleepiness, confusion and impulse control disorders, such as uncontrolled shopping, gambling, eating and sexual urges. Studies show 28% of people with Parkinson’s stop taking dopamine agonists due to side effects, while 40% need to add another medication within two years.
Levodopa: Levodopa, the most effective drug for Parkinson’s movement symptoms, replaces dopamine in the brain. It is usually given in combination with the drug carbidopa to reduce nausea, a common side effect. Taking levodopa with meals can also reduce nausea, but protein may interfere with the drug’s effectiveness. About 2% of people taking levodopa stop due to side effects, while 15% need to add another medication within two years.
Dyskinesia, also linked to levodopa, can often be managed by a dose adjustment or through direct treatment, using a medication called amantadine. It works by blocking NMDA, a chemical that causes extra movement. Immediate-release amantadine is also sometimes used alone for Parkinson’s movement symptoms. There is an increased risk of confusion and hallucinations with amantadine use in people over 75. It can also be associated with leg swelling, skin changes and other side effects.
Anticholinergics: The medications trihexyphenidyl and benztropine are sometimes used to improve tremor or dystonia — painful, sustained cramping . They work by blocking acetylcholine, a brain chemical tied to movement. However, their use should be avoided in people 70 and older due to the risk of confusion and hallucinations. Anticholinergics can also be associated with blurred vision, dry mouth, constipation and urinary retention.
Medications your doctor might consider to improve the effects of levodopa include:
MAO-B inhibitors: Monoamine oxidase-B inhibitors rasagiline, selegiline and safinamide make more dopamine available to the brain. These medications can be used alone or in combination with levodopa to extend effectiveness. MAO-B inhibitors are generally well tolerated, but 70% of people taking them alone for Parkinson’s will need to add another medication within two years.
COMT inhibitors: Medications such as entacapone and opicapone increase available levodopa in the brain by blocking the catechol-O-methyl transferase enzyme.
A2A receptor antagonist: Istradefylline, an adenosine A2A antagonist, blocks adenosine at A2A receptors in the brain to reduce levodopa “off “time.
Inhaled levodopa is often used with levodopa, as needed, for sudden “off” time. Injectable apomorphine can also be used on demand, for “off” time relief. Both medications can increase the risk of dyskinesia.
It is important to work with your doctor to find the right balance for you. Your doctor might increase or decrease your levodopa based on your symptoms. For example, tremor, stiffness or mobility issues might benefit from an increase in levodopa. However, hallucinations, confusion and low blood pressure might improve with a decrease in levodopa.
There are also strategies and medications to manage drooling, runny nose, sleep issues, gut issues, thinking changes and other Parkinson’s challenges.
What if levodopa doesn’t seem to be working?
If you are taking levodopa but aren’t seeing benefits, talk to your doctor. Here are some questions to ask:
- Is the symptom troubling you one that doesn’t respond well to levodopa? Could it be related to another health issue?
- Would you benefit from a referral to a rehabilitation therapist or another health professional?
- Could something be interfering with how your body is absorbing medication? Some people experience less benefit when taking levodopa with a high-protein meal.
- Do you have a condition that mimics Parkinson’s?
It is also important to discuss whether your dose needs to be adjusted. For example, the effects of Sinemet, a form of levodopa, only last a short time — after 90 minutes half of it is gone. Your doctor might adjust the timing and dose of levodopa, use a longer-acting formulation or recommend taking your medications 30 minutes before or 60 minutes after eating a meal.
Advanced Therapies
If it becomes difficult to control motor fluctuations by adjusting oral medications, there are other options to improve medication absorption and reduce “off” time:
-
Duopa therapy delivers carbidopa-levodopa gel directly to your intestine through a surgically placed tube.
-
Foscarbidopa and foslevodopa (Vyalev) therapy uses a pump to steadily deliver a form of levodopa under the skin through a small tube called a cannula. A needle is used to place the cannula.
-
Continuous apomorphine therapy (Onapgo) uses a pump to deliver continuous apomorphine through a fine needle placed under the skin.
These medications require lifestyle adjustments, training to use and a commitment to good skin care to reduce the risk of irritation and infections.
Options Beyond Medication
More advanced Parkinson’s symptoms can sometimes benefit from other treatment strategies, such as deep brain stimulation (DBS) — which involves surgically implanting an electrical pulse generator connected to electrodes placed in the brain to address Parkindeep-brainson’s movement symptoms and some non-movement symptoms.
DBS might be considered for someone who:
-
lives with classic Parkinson’s disease
-
has symptoms that respond to levodopa
-
experiences frequent motor fluctuations and tremor, despite consistent medication dosing
-
has bothersome dyskinesia
Following DBS, many people can reduce their medications and still experience a reduction of their PD symptoms. The reduction in dose of medication can lead to decreased dyskinesia.
Focused ultrasound, a non-invasive therapy, does not require a surgical incision. During the procedure, high-frequency sound waves are aimed at a specific area of the brain connected to tremor to relieve Parkinson’s tremor. Unlike DBS therapy, which is adjustable and reversible, focused ultrasound changes are permanent.
If you have questions about PD treatment options, contact our Helpline at 1-800-4PD-INFO (473-4636) or Helpline@Parkinson.org.
Learn More
Explore our resources about medications to treat symptoms of Parkinson’s:
-
Download our book Medications: A Treatment Guide to Parkinson’s Disease
Related Materials
Pain in Parkinson's Disease
Occupational Therapy and PD
Nutrition and PD
Related Blog Posts


Shaping the Future of Parkinson’s Policy: Meet Our Chief Strategy and Policy Officer