GBA Mutation May Lead to Novel Therapeutics

One of the most common genetic risk factors for Parkinson’s disease (PD) is having a mutated GBA gene (which makes the enzyme glucocerebrosidase). In fact, 5 to 10 percent of people with PD have that specific GBA mutation in one copy of the gene (mutations in both copies of the gene lead to Gaucher disease). It is more common than other genetic mutations associated with PD such as LRKK2, α-synuclein (SNCA) and PARK2. People with PD who have the GBA mutation tend to experience motor symptom deficits sooner, cognitive decline more rapidly and have particular difficulty with their gait (walking) and postural balance.
When GBA works as it should, it helps code (provide instructions) for making a digestive enzyme that breaks down potentially harmful substances, getting rid of unwanted bacteria and performs various housekeeping duties, including recycling worn out cell components. If both copies of the GBA gene are damaged (mutated), this negatively impacts a cascade of essential processes — which can lead to a dangerous build-up of toxins that harm the spleen, liver, lungs, bone marrow and brain (Gaucher disease). To date, most studies assessing GBA-related PD risk have been performed primarily in European and Asian-derived populations, while very few studies have been done in other populations, such as in the Latino population of South America.

A recently published study, titled, “The distribution and risk effect of GBA variants in a large cohort of PD from Columbia and Peru” (Velez-Pardo et al., 2019) sought to remedy that shortfall and characterize the frequency and distribution of GBA variants (variations in the gene). Specifically, Valez-Pardo et al. (2019) sequenced the entire GBA coding region in 602 participants with PD and 319 controls (people who do not have PD) from Colombia and Peru — all of whom were enrolled in the Latin American Research Consortium on the Genetics of Parkinson's disease. Age at enrollment was comparable for all participants. All study participants were evaluated by a movement disorder specialist at each site and met UK PD Society Brain Bank criteria for PD. The study used a blood test to sequence DNA from each participant.
Results
- A significantly higher proportion of GBA mutation carriers (mutation in one copy of the gene) were seen in people with PD compared to people without Parkinson’s.
- Those with GBA mutations from Peru and Columbia have a 4- and 6-fold increase in PD risk, respectively.
- The age at onset was significantly earlier in GBA carriers (about 8 years) when compared to people with PD who were non-carriers.
- A novel population-specific GBA mutation called, p.K198E was found only in Colombian participants. This was the first study to identify the p.K198E mutation.
- Frequency of GBA mutations in Colombian participants was more than double most populations, e.g., Peruvian participants and European-derived populations. Note: This was primarily due to the presence of a population-specific mutation, p.K198E.
What Does It Mean?
While the specific biological mechanisms are still unclear, this study found that genetic changes in the GBA gene is linked to a higher risk of developing PD in both Columbians and Peruvians. Further, the novel mutation (p.K198E) the authors identified, found exclusively in the Columbian population, suggests there may be more yet to be discovered mutations in Latin American populations, that could provide unique insights into the disease mechanism.
Moreover, as nearly 10% of the Columbian population carries the GBA mutation — as opposed to about only 4% in other populations — the Columbian PD population may be particularly well suited as a group to study novel therapeutic approaches targeting GBA-related PD.
Learn More
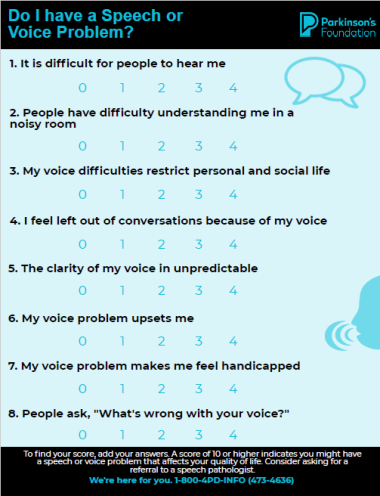
The Parkinson’s Foundation believes in empowering the Parkinson’s community through education. Learn more about GBA and common PD mutations by vising the below Parkinson’s Foundation resources or by calling our free Helpline at 1-800-4PD-INFO (473-4636) for answers to all your Parkinson’s questions.
Related Blog Posts

Treating Sleep Apnea May Lower Parkinson’s Risk

Top Parkinson’s Science News Articles of 2025