Parkinson’s & the COVID-19 Vaccine

Two new COVID-19 vaccines are currently in distribution across the U.S. with several others in production across the globe. Collectively, these vaccines are bringing hope and excitement to the millions of Americans, including those with Parkinson’s disease (PD), who are actively protecting themselves from exposure to the virus. Both vaccines available in the U.S. provide some protection in the event of a COVID-19 exposure and help the body more rapidly clear the infection.
On January 7, Michael S. Okun, MD, Parkinson’s Foundation National Medical Advisor, led a Parkinson’s Foundation Facebook Live event, “Parkinson’s & the COVID-19 Vaccine.” Dr. Okun answered the PD community’s most pressing questions about the vaccine.
“If you have Parkinson’s, you should get the COVID-19 vaccine,” Dr. Okun said. “The benefit is really high and favors receiving the vaccine as soon as possible. It is in the best interest for all persons with Parkinson’s disease to pursue the vaccine as soon as it is available in the region you live. Of course, talk to your doctor first as there are a handful of rare exceptions for those who cannot receive the vaccine.”
Question: How does the COVID-19 vaccine work?
Dr. Okun: When the COVID-19 vaccine goes into the body, it tells your immune system to make antibodies (proteins that identify and attack the identifying marker of the COVID-19 virus) to fight COVID-19. Antibodies bind, like a lock and key, to viruses and other threats. The vaccine does not prevent COVID-19 infection but it does teach your immune system what COVID-19 looks like and how to attack it if you are infected.
To achieve its optimal effectiveness, you will need to get both doses of either vaccine. Both vaccines available in the U.S. (produced by Pfizer and Moderna) have identical effectiveness. They use a new treatment approach called messenger RNA (or mRNA), which send a message into the building blocks of your cells and body — the message stimulates a response and stimulates antibody production to create a COVID-19 defense system.
Should all people with Parkinson’s disease get the vaccine?
Dr. Okun: Yes. I recommend this vaccine to all my patients with Parkinson’s in my medical practice. Movement disorder specialists have largely agreed as a global recommendation that everyone with PD should get this vaccine, with few exceptions. This is an incredibly safe vaccine. I have lost patients to COVID-19. This virus can be preventable, but it will take more than just the vaccination. We must follow the three C’s:
- Cover. Always wear a two- or three-ply face mask (like a surgical mask) when you are around others or in public. Don’t wear bandanas or gaiter face coverings.
- Control. Control your environment. If necessary, interact with others outdoors while maintaining a distance.
- Contain. Minimize gatherings. Walk or sit six feet or more away from one another. Do not trust anyone who does not live full time in your home.
Can you still get the COVID-19 infection after you get the vaccine?
Dr. Okun: Yes. Even after being vaccinated, you can still be infected with COVID-19, spread it and experience COVID-19 symptoms. In most cases we are predicting that the symptoms will be less severe. The data also strongly suggests that COVID-19 is much less likely to be deadly after receiving two shots of the vaccine.
Do I still need to wear a mask If I get the COVID-19 vaccine?
Dr. Okun: Yes. You still need to wear a mask and keep at six- to 12-foot distance after receiving the vaccine. We are still seeing high numbers of the virus spreading among people who are in public and do not protect themselves. If you get the vaccine, you can still be infected with COVID-19, and spread it. If you do not wear a mask you could spread the virus to someone else without even knowing it, and this could have serious health consequences for others — especially the elderly and at-risk groups. Remember to cover, control and contain.
If I get the vaccine can I see my children or grandchildren?
Dr. Okun: Maybe, it depends on many factors. If you decide to see your grandchildren, wear your mask and follow the three C’s. If you do not live with them and you receive the vaccine (both shots), we still recommend masking, staying outside and keeping six to 12 feet apart. The safest situation remains seeing only people who live in your house. Be aware that children who attend in-person schooling may have many exposures.
If I had COVID-19 should I still get the vaccine?
Dr. Okun: Yes. The Centers for Disease Control and Prevention (CDC) recommends waiting a few weeks after you recover from COVID-19. At UF Health, we have health professionals who have contracted COVID-19 and were vaccinated. We do not know if having COVID-19 will help you develop and maintain the antibodies necessary to fight off the disease. Risk and mortality are so high with this virus that we recommend receiving the vaccination as soon as you can after infection with COVID-19. Following current CDC guidelines, most doctors wait several weeks after infection before vaccination.
Are there side effects from the vaccine?
Dr. Okun: Side effects are mostly local and occur in the region of the injection (the shoulder in most cases). The vaccine goes into the muscle and works up your immune system (we recommend receiving it in your non-dominant arm). The most likely side effect you may experience is a sore arm for a few days, with complete use of the arm.
When you return for your second shot, about half of people will experience mild to moderate flu-like symptoms and possibly a fever for a day or two — try to avoid work or public places for those days if you can. This adverse reaction is a good thing. It is a sign that your immune system is working hard, NOT that you have COVID-19.
Relatively common side effects include:
- Pain at injection site
- Fatigue
- Headache
- Muscle pain
- Chills
- Joint pain
- Fever
- Injection site swelling
- Injection site redness
- Nausea
How can I access the vaccine?
Dr. Okun: In the U.S., the vaccine is being distributed to each of the 50 states, and each state has a different process for distribution. In most states, the vaccine is currently being administered to frontline healthcare workers, and eventually it will be distributed by age and priority levels. Tips to access the vaccine include:
- Check in with your local health department. Some have a sign-up list so that you can access appointments online or by calling.
- Check in with your primary doctor and let him/her know you want the vaccine.
- Call nearby hospitals and ask them about their distribution plan and whether you can receive it there.
- Don’t wait in line for hours or camp out without social distancing. Ideally, get an appointment.
We are working on getting people with Parkinson’s to be listed as a 1b priority, meaning they would get priority in receiving the vaccine. If it were up to me, I’d be vaccinating everyone with Parkinson’s disease early in the process (regardless of age), and I’d do it tomorrow.
Guidance on who will receive the COVID-19 vaccine at each stage of the rollout is determined at the state level. Contact your state’s health department for details about when you and your loved ones will be eligible to receive the COVID-19 vaccine. Find your state’s health department.
We are hearing that in some areas, if you communicate to your doctor, healthcare system and local health department that you have Parkinson’s you may possibly be offered the vaccine earlier (regardless of age). There is no harm in asking and also informing the local authorities about your condition.
What do people with Parkinson’s need to bring with them for their vaccine appointment?
Dr. Okun: Take your personal information (identification) and medication list. If you are prone to fainting, let the nurse know. For the second shot, bring the card issued to you on the first shot, so that the vaccine administration can be documented. Take a picture of the card once you have both shots so that you always have a copy.
I have Parkinson’s and blood pressure issues. Should I be worried about getting the vaccine?
Dr. Okun: No. You will most likely be sitting when you get the vaccine, so if you get faint or have a change in your blood pressure you should be okay. Stay hydrated; it will help with changes in blood pressure. Take a water bottle and a snack with you. You will likely be asked to sit in a waiting area for 15-20 minutes after each shot to make sure you do not have a reaction. If you can drink a small bottle of water either immediately before or immediately after the shot, we believe this is a good idea, especially if prone to fainting.
What are the differences between available vaccines?
Dr. Okun: Moderna and Pfizer vaccines are distributed in the U.S. and in other countries, with 94 and 95 percent effectiveness. Both require two dosages and need to be stored at incredibly low temperatures — the Pfizer vaccine requiring an even lower storage temperature than the Moderna vaccine — making distribution and storage a challenge. These two vaccines belong to a new treatment approach called messenger RNA (or mRNA) vaccines, which create a COVID-19 defense system.
Other vaccines are in development around the world and most work more like a traditional vaccine (like the flu vaccine). They send instructions through DNA, teaching the immune system how to respond to COVID-19. There are several vaccines in early development, but these have the most available information:
- Oxford–AstraZeneca: distributed in the U.K. with ~70 percent effectiveness. It works in two dosages. The major benefit to this vaccine is that it can be stored at refrigerator temperatures. The vaccine may be more effective (~90%) if a weakened first shot is followed a few weeks later by a standard dose.
- Sinovac and Sinopharm: created in China with ~78-80 percent effectiveness using two dosages. There is limited data on these vaccines. Sinovac is currently in late-stage trials in other countries.
- Sputnik V: distributed in Russia and works using two dosages. Early reports are of ~92 percent effectiveness. However, there is limited data on this vaccine.
Overall, if we could decrease the refrigeration requirements and lower the cost of production, we can distribute the vaccine worldwide. The Oxford-AstraZeneca vaccine is the leading candidate for worldwide distribution.
I’m allergic to other vaccines, should I get the COVID-19 vaccine?
Dr. Okun: In many cases, people with allergies to vaccines may possibly receive the Moderna or Pfizer vaccines. Side effects including allergies to vaccines are usually caused by the fluid surrounding the vaccine itself. Do not assume you cannot get this vaccine; talk to your doctor. Old fashioned vaccines are manufactured in a completely different fashion as compared to the current COVID-19 vaccinations. It will be rare for someone to not be able to receive the vaccines; we believe most people are eligible.
If I had Guillain-Barré syndrome in the past, can I get the vaccine?
Dr. Okun: In rare cases, among both children and adults, a bad reaction to past vaccines could result in Guillain-Barré syndrome — a condition where the immune system attacks nerves in the body, resulting in loss of sensation, muscle weakness and in some cases temporary paralysis. This syndrome usually resolves in several weeks/months. We are NOT however seeing Guillain-Barré associated with the COVID vaccine as was shown by a recent study. A history of Guillain-Barré syndrome does NOT mean you should avoid receiving the vaccine. If you just recovered from Guillain-Barre syndrome however, most experts recommend you should speak with your doctor and wait a few weeks before vaccination.
Dr. Okun also answered questions about COVID-19 and Parkinson’s:
Is it more difficult to recover from COVID-19 if you have Parkinson’s?
Stay up to date with Parkinson's and COVID-19 information at Parkinson.org/COVID19.
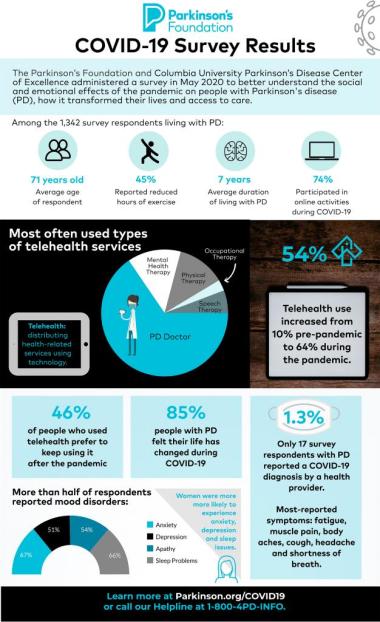
Dr. Okun: Data suggests that having Parkinson’s means a more difficult COVID-19 recovery. Since this virus is still actively spreading, we are collecting tons of data on COVID-19 patients. A study from The Roy J. and Lucille A. Carver College of Medicine at the University of Iowa, a Parkinson’s Foundation Center of Excellence, showed that people with Parkinson’s who contracted COVID-19 had a 30 percent increased risk of mortality (death) from the virus.
If someone did not have Parkinson’s before, is it likely that they will develop it after recovering from COVID-19?
Dr. Okun: We do not have the numbers on how common it is to receive a Parkinson’s diagnosis after recovering from COVID-19. There are several intriguing papers on how COVID-19 may affect the brain and how it may possibly contribute to Parkinson’s risk. At this point, we caution the public and researchers not to speculate until we have more data.
What are the most common COVID-19 symptoms people with Parkinson’s experience?
Dr. Okun: We are just starting to get the information on clinical Parkinson’s symptoms and COVID-19. One study in Milan, Italy, reported that motor and non-motor symptoms seemed to worsen with COVID-19, and that medication adjustments were required in a third of people with PD and COVID-19. Researchers hypothesized that the COVID-19 infection, the Parkinson’s medications, and the immune system, together create a perfect storm to worsen Parkinson’s symptoms. The most common symptoms encountered were urinary issues, fatigue, cognitive dysfunction and confusion. We are seeing many patients who survive COVID-19 and require that their PD medications be adjusted. Similarly, we are also finding that in the hospital, a neurologist with expertise in Parkinson’s can help in decision making for those with COVID-19.
Can COVID-19 cause dementia in the long-term?
Dr. Okun: We do not know. Researchers will be studying this virus for many years to come. There have been studies linking the virus to post-recovery neurological symptoms, but we will need more data and more studies to answer this question.
Do people with Parkinson’s get priority access to the COVID-19 vaccine?
Each state has its own process for rolling out the vaccine to different population groups. If you would like to advocate for people with Parkinson’s to be part of a priority group, we encourage you to contact your elected officials.
More Information:
- COVID-19 and Parkinson’s: Parkinson.org/COVID19
- CDC: COVID-19
- CDC: COVID-19 Vaccines
- U.S. Department of Veterans Affairs: Program of Comprehensive Assistance for Family Caregivers (PCAFC)
We’re here for you. For Parkinson’s information, references to online programs and local resources, please contact the Parkinson’s Foundation Helpline at 1-800-4PD-INFO (473-4636).
Related Blog Posts


Start 2026 Strong: Simple Resolutions for Better Health