My PD Story

John Rosiak
When I was diagnosed with Parkinson’s disease (PD) in the fall of 2023, my response was to go on a crash course to learn as much as I could about this “progressive” disease and see what action I could take.
I was familiar with the disease, trying to help support my brother’s journey with PD the last 10 years of his life. I saw his classic symptoms of slowness, falling, freezing, swallowing and speech problems, and more. Yet, he never really had tremors, and his mind was sharp until the end. I didn’t understand just how different PD can be in different people.
A few years ago, I was constantly fatigued and losing confidence in my balance. I went to my primary care physician (PCP), who sent me to different doctors to find the underlying problem. These referrals included a neurologist, who ordered an MRI, and did the standard “clinical assessment.” She said I didn’t have PD.
The cardiologist, sleep study, endocrinologist, and ear, nose and throat (ENT) specialists, all found no answers to my symptoms. So, back to the PCP, who told me to avoid the heat, and referred me to another neurologist, which took months to get an appointment.
This neurologist made the clinical diagnosis of Parkinsonism. To learn more, she offered me a choice of a skin biopsy to see if there was alpha synuclein abnormality, or a DaTScan, to see if there was any dopamine deficit. I chose the former. When the synuclein skin biopsy test came back abnormal, that “supporting information” warranted the diagnosis of PD in December of 2023, even though symptoms were mild.
I immediately went to clinicaltrials.gov to see what studies I should sign up for, thinking I could learn more about my new situation, and how to get a handle on it. I am fortunate to live in the Washington, DC area, with its abundant biomedical centers and institutions. I applied to the Parkinson’s Progression Markers Initiative (PPMI) study, which included a DaTScan at Johns Hopkins Parkinson's Disease and Movement Disorders Center, which is also a Parkinson’s Foundation Center of Excellence.
My neurologist later read that DaTScan, which showed an overall loss of dopamine in my brain, and a more significant loss of dopamine in the right brain hemisphere. This scan helped explain why I had less coordination and strength on the left side of my body. The positive DaTScan result provided further “supporting” information for the diagnosis of PD.
I signed up for the National Institute of Health’s (NIH) Phenotype/Genotype Correlations in Movement Disorders, run out of their Parkinson’s Clinic. My wife and I spent a day there meeting with neurologists who tried to understand my case, given the mild symptoms. They also drew blood to test the full genome to check for PD-related genes.
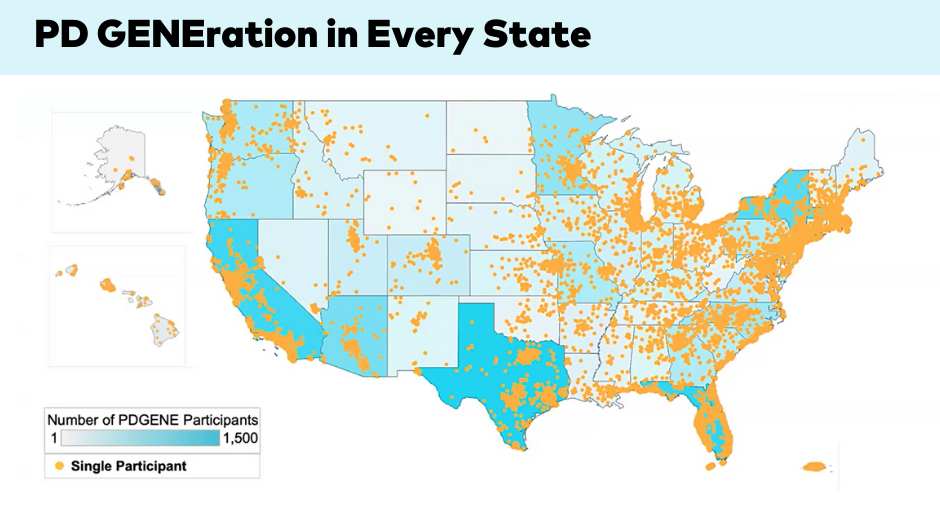
I also signed up for the PD GENEration: Mapping the Future of Parkinson’s disease genetic testing study, which collected my genes by a buccal (cheek) swab. The results were back in one month; they were negative for any of the seven genes related to PD. That testing came with excellent genetic counseling to understand what the results meant for my family and me. Likewise, NIH’s genetic testing “did not detect disease-causing variants.” I was interested to know if there was a genetic connection because I figured that might tell me something about possible disease progression, and preferred treatments.
There was one more study I signed up for right away. In December of 2023 I contacted Marymount University in VA, about participating in their study about the effects of rock climbing on PD. I signed up for data collection in January, which involved 10 baseline measures that assessed agility, balance, grip strength and general well-being. Then I had to rock climb 24 times in 12 weeks.
I finished all 24 climbs by March. I then repeated the 10 tests I took in January, before climbing. I didn't see the comparison results (it's a study, so it was “blind”), but I really feel that I did as well on the posttests, or even better, after all those climbs, than on the pretests back in January.
I never did rock climbing before, but did many other physical activities over the years. I knew that exercise was so important for PD, as well as for general health. In January I told my wife, "I hope I like rock climbing because I just signed up to do 24 climbing sessions in 3 months!" After climbing for several months for the study I have to say I don't like rock climbing — I love it!
Exercise in the form of climbing has changed my life. After every session my body feels tired and sore (which, frankly, I feel all of the time with PD). But I liken that feeling to those good, tough workouts from playing sports for years. Walking out of the climbing gym I feel better. That natural dopamine my brain is short of might be kicking in because of the climbing. I walk with greater confidence. My attitude toward life is positive and focused. I forget about the PD.
I continued to climb the rest of the year (in fact, I now work at the gym instructing others). In addition to climbing twice a week with my peers with PD in the UpENDing Parkinson’s program I try to help support UEP’s growth so more climbers in more gyms can participate in this remarkable exercise therapy.
In addition, I completed the Parkinson’s Foundation Ambassador training, and was also trained as a Research Advocate. I continue to look for, and participate in a variety of studies, many of them online, run by various universities or institutions trying to understand various issues related to PD.
I believe research is so important to help people better understand the disease and, more importantly, what we might be able to do about it.
My goal is to be as active as I can physically and mentally. Having the diagnosis has also prompted more reflection about life. While not sure what the future will bring, I am grateful to have found a “power through weakness.” Because of this experience, I have a new perspective, and hope for the future. There are so many resources to help those living with PD.
Explore how you can get involved in Parkinson’s research today. Visit our Join A Study page and learn more about our Research Advocate program.
Related Materials
Pain in Parkinson's Disease
Occupational Therapy and PD
Nutrition and PD
More Stories
from the Parkinson's community