Parkinson’s Foundation Presents Five Findings at International Congress of Parkinson’s Disease and Movement Disorders®

Every year thousands of Parkinson’s disease (PD) experts and researchers share research findings that have the potential to help people living with Parkinson’s at the International Congress of Parkinson’s Disease and Movement Disorders. This year the conference took place from September 27 to October 1 in Philadelphia, PA.
The Parkinson’s Foundations shared five new Parkinson’s studies, revealing new information about genetics research, care and our work with the Black and African American community. These findings offer new hope for people living with PD and caregivers alike.
Explore the five research findings the Parkinson’s Foundation shared with the international PD community below:
1. Expanding the PD Generation Study to Increase Clinical Genetic Testing and Counseling Using Whole Genome Sequencing Among Diverse Parkinson’s Populations
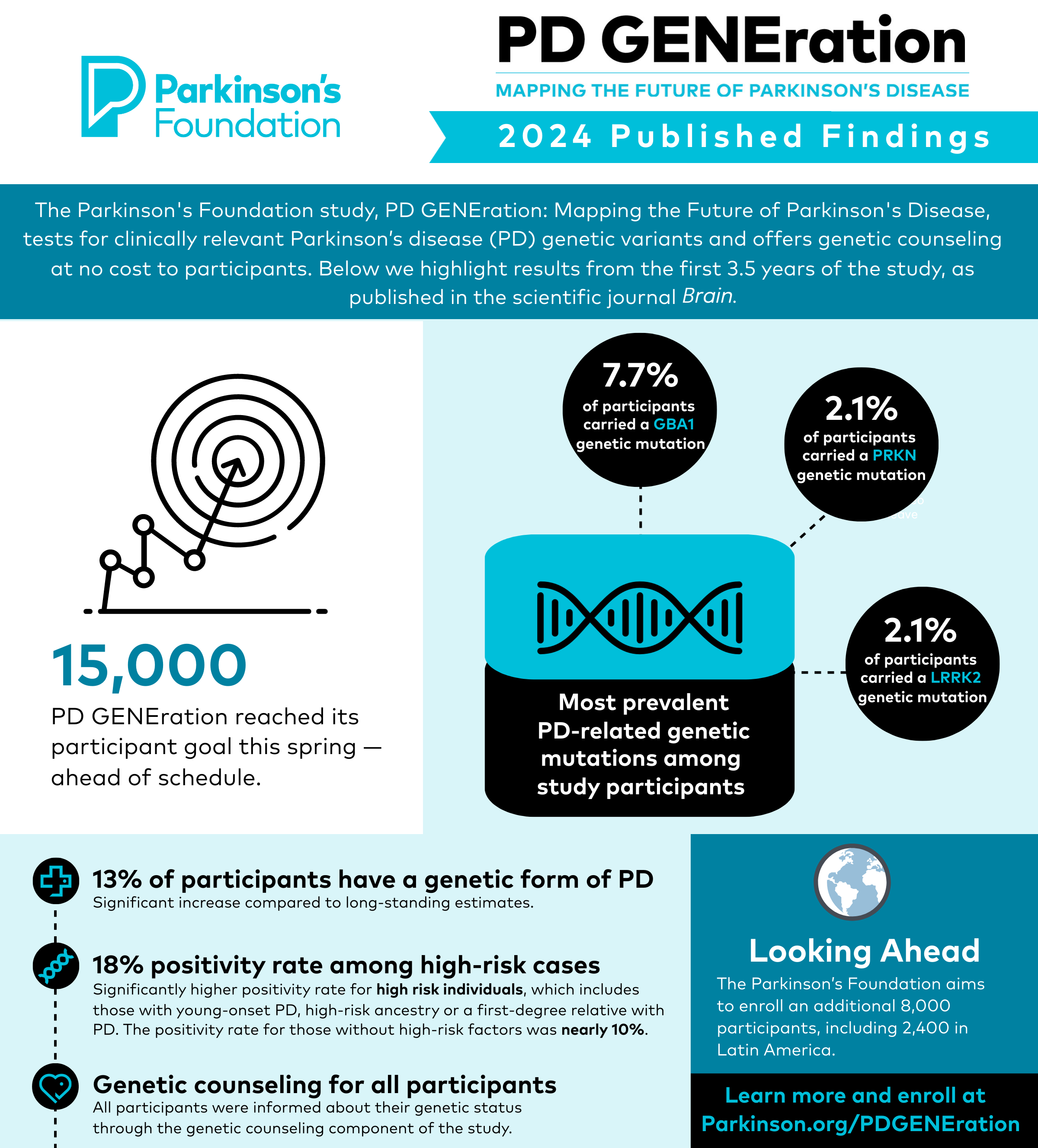
PD GENEration: Mapping the Future of Parkinson’s disease is a Parkinson’s Foundation research study that offers genetic testing and counseling, in English and Spanish, to people with Parkinson’s through a whole genome sequencing platform. This study aims to simplify access to clinical genetic testing to people with PD and offer educational materials to clinicians on PD genetics.
Key Takeaways:
-
The study has enrolled 18,003 participants, as of September 2024.
-
The study has expanded to five countries from Latin America (Colombia, Chile, Peru, Mexico, Ecuador), Israel, Canada, and 10 additional sites in the U.S. that focus on underrepresented populations.
-
12.2% of people with Parkinson’s, who have completed testing, tested positive on the PD GENEration 7-gene panel.
-
By providing genetic testing to all those interested and from all backgrounds, the study helps inform care, diversify the data, help engage people in research, and qualify more for enrollment in clinical trials for PD.
PD GENEration goals include helping accelerate clinical trials in PD, improving PD care and research and empowering people with PD and their care teams.
Learn more & enroll in PD GENEration.
2. Engagement of the Black and African American Community in PD Genetics Research
Advancements in understanding the biological pathways of Parkinson’s have largely been focused on people of European ancestry. There is a critical need to understand genetic differences across populations, including people with African ancestry. The Parkinson’s Foundation partnered with Morehouse School of Medicine, a historically Black institution of medicine to improve inclusion in PD GENEration, prioritize PD awareness, education and resources; and tailor our research advocacy training program — the Learning Institute.
Key Takeaways:
-
Through this partnership with Morehouse School of Medicine, from November 2021 to March 2024, 157 Black and African American participants enrolled in PD GENEration.
-
14 community education events were held, including the Learning Institute in September 2023.
-
Media was developed and utilized to expand reach and included two webinars, five podcasts and six blogs/news articles.
Establishing partnerships with trusted sources of the Black community is critical to providing equitable access to PD education and resources, including PD GENEration. Focusing on diversity and inclusion in PD GENEration will accelerate breakthroughs towards a cure for PD.
Learn more about our impactful partnership with Morehouse.
3. Benefits of Parkinson’s Team Training Are Maintained Long-term
The goal of Parkinson’s Foundation Team Training is to provide more coordinated and complete patient-centered care to improve the quality of life of people with PD and caregivers. Our study aimed to demonstrate the effectiveness of the training program and determine if the benefits of Team Training are maintained long-term.
Key Takeaways:
-
Through Team Training, team members become more effective in delivering better interprofessional, patient-centered care.
-
Results showed significant and sustained improvements in:
-
Healthcare professional confidence in various measures of providing care
-
Team coordination working with persons with PD and their care partners
-
Understanding of the other team member roles and how team members can assist in the care of persons with PD and their care partners.
-
The effectiveness of the Team Training program’s education is maintained and sustained long term. Better care leads to better lives for those living with PD and their care partners.
Parkinson’s Foundation Team Training provides a continuing education program for healthcare professionals to learn more about PD and how to develop and maintain an effective PD interprofessional team.
Explore our Learning Lab courses, designed for healthcare professionals.
4. Engage, Educate and Empower: Parkinson’s Research Advocates from the Black and African American Community
Black and African American people with Parkinson's face significant disparities in care, including delays in diagnosis and treatment, limited access to care and historical exclusion from research. To address these challenges, the Parkinson’s Foundation Research Advocacy Training program, the Learning Institute, was tailored to engage, educate, and empower the Black community in Parkinson’s research.
Key Takeaways:
-
The Learning Institute was held in September 2023. 33 people from the Black community were trained in research advocacy.
-
Many research advocates felt prepared to begin research advocacy (79%) and most felt excited about the work they can do as a research advocate (83%).
-
To date, 17 advocacy tasks were completed by 26 research advocates, including presentations at local churches and health fairs, panelists at a Parkinson’s Foundation community-based program, and partnerships with researchers.
The Learning Institute empowered African Americans living with PD to become advocates for community outreach and engagement. This program has the potential to drive meaningful change, enhance health equity, and improve outcomes for those living with PD in the Black and African American community.
Learn more about our research advocates.
5. Hospital Care Learning Collaborative: Sharing Strategies to address the Parkinson’s Foundation Inpatient Clinical Care Standards
With the launch of the Parkinson’s Foundation Hospital Care Learning Collaborative, the Foundation in partnership with healthcare leaders, clinicians and institutions, aims to eliminate preventable harm and promote higher reliability in care for people with Parkinson’s in the hospital. The Learning Collaborative work to implement quality improvement projects focused on improving hospital safety for people with PD. Participants shared strategies and best practices to address the hospital care standards, as outlined in the Parkinson’s Foundation Hospital Care Recommendations.
Key Takeaways:
-
A framework to work with the hospital IT team to request adjustments to the Electronic Health Record, including the ability to customize times for Parkinson’s medication orders.
-
Strategies to avoid medication delays in the event of safety concerns due to swallowing challenges (dysphagia), including the use of crushed Parkinson’s medication and an automated trigger for a Speech Language Pathologist evaluation.
-
The use of an Electronic Health Record alert when unsafe medications are ordered, offering alternatives that are already approved by the hospital Pharmaceutical & Therapeutics committee.
The Parkinson’s Foundation is committed to improving hospital safety for people with PD. In addition to our Hospital Safety Guide, a resource for people with Parkinson's and care partners, the Foundation works with hospitals and health systems to help promote awareness and delivery of the best care for the Parkinson’s community.
Read and download the Hospital Safety Guide today.
Stay up to date with Parkinson’s Foundation through our Parkinson’s Today blog.
Related Materials
Related Blog Posts

Mapping the Brain in High Resolution: How the University of Michigan is Advancing Parkinson’s Neuroscience

Top Parkinson’s Science News Articles of 2025