We Answer the Most Frequently Asked Parkinson’s Foundation Helpline Questions

To offer more support to the nearly one million people in the U.S. living with Parkinson’s disease (PD), the Parkinson's Foundation has expanded its Helpline hours. You can call with the Helpline with your PD questions at 1-800-4PD-INFO (473-4636), in English and Spanish, Monday through Friday from 9 a.m. to 7 p.m. ET.
The Parkinson’s Foundation Helpline provides guidance on:
- current disease information
- medical issues including symptoms and treatments
- health and social care
- emotional support
- referrals to local health professionals
We recently asked the trained Parkinson's information specialists who answer Helpline calls to share the answers to the most frequently asked questions below. If you have a question that is not listed below, please call our Helpline!
Q: Can the Helpline provide me with Parkinson’s specialists, exercise classes and support groups?
A: Yes. The Helpline can provide names of Parkinson’s movement disorder specialists, neurologists and other Parkinson’s specialists — like a physical therapist, occupational therapist, speech therapist and more — in your area. Helpline specialists can also provide nearby exercise classes and support groups.
Q: Is there a special diet that can help with my Parkinson’s?
A: A balanced, nutritious diet is important in Parkinson’s. The best plan is to maintain a full diet with all the daily nutritional requirements — try to eat lots of fruits and vegetables, lean proteins and whole grains. Many doctors recommend the Mediterranean diet for its ability to help reduce blood pressure and cardiovascular disease. Also, try to drink plenty of water to help with constipation.
Q: My family member told me about a vitamin/supplement/tea that can relieve PD symptoms. Does it work?
A: Many people add vitamins to their treatment regimen, incorporating antioxidants such as vitamin B6, vitamin E, vitamin C, Coenzyme Q10, glutathione, in the hope of slowing the disease. Be wary of new supplements that claim to cure multiple symptoms, as they often lack rigorous testing. Since Helpline specialists stay up-to-date on PD treatments, call to discuss any supplement you hear about.
Q: Should I not eat protein when I take carbidopa/levodopa (brand name Sinemet)?
A: Most people who are newly diagnosed will not have a problem. For some people, particularly those living with PD for many years, eating protein-rich foods limits the effectiveness of levodopa. Most people who have trouble with Parkinson’s related to a diet high in protein report that their medications are not working. Levodopa works best when taken on an empty stomach. Taking it 30 to 45 minutes before eating can help.
Q: As the primary caregiver, I find myself frequently feeling overwhelmed and unable to keep up with my own needs. What should I do?
A: Up to 70 percent of caregivers are significantly stressed and half meet the criteria for clinical depression. Take immediate action when you find you are ignoring your own needs, feel isolated, experience anxiety, resentment, demoralization or depression. Try to alleviate caregiver stress by recruiting friends and family or hiring a paid caregiver to help with care. Don’t wait, and get help managing caregiver-related anxiety, stress or depression by seeing a psychologist or therapist. Remember that you need to take care of yourself to be well enough to take care of others.
Q: Is there financial assistance available for people with Parkinson’s?
A: While the Foundation does not give financial aid, Helpline specialists provide referrals to organizations that may be able to help with financial assistance for medication, transportation, basic needs and respite or nursing home care. A good place to start is to locate your nearest Area Agency on Aging office through the Eldercare Locator Service for help finding financial aid and related programs. Our specialists can also give information about various government social service programs.
Q: What other therapies can help with my Parkinson’s symptoms?
A: A comprehensive and multi-disciplinary approach to health care can be very beneficial at any stage of Parkinson’s. Building a healthcare team involves taking advantage of not only the expertise of a PD specialist, but the help of a physical therapist, occupational therapist, speech therapist, nutritionist, social worker and others. Some may be able to find all of these professionals in one practice or center, but many will have to explore their community’s resources.
While we are happy to discuss any issue with you, calling our helpline is not a substitute for seeing a doctor.
No one should have to face Parkinson’s alone. Call the Parkinson’s Foundation Helpline today at 1-800-4PD-INFO (473-4636) or email us at Helpline@Parkinson.org with your Parkinson’s questions in English or Spanish.
Related Blog Posts

20 Parkinson’s-Friendly Gifts

8 Tips for Traveling with Parkinson’s


 However, we still don’t have biomarkers, such as a blood test, that allows us to assess PD progression and test promising therapies in people with PD. Therefore, our best opportunity to test a new potential disease modifying therapy is to see if it can slow progression of PD signs and symptoms in people who were recently diagnosed with early PD and who are not taking symptomatic medications (like levodopa, dopamine agonists, amantadine, or MAO-B inhibitors).
However, we still don’t have biomarkers, such as a blood test, that allows us to assess PD progression and test promising therapies in people with PD. Therefore, our best opportunity to test a new potential disease modifying therapy is to see if it can slow progression of PD signs and symptoms in people who were recently diagnosed with early PD and who are not taking symptomatic medications (like levodopa, dopamine agonists, amantadine, or MAO-B inhibitors). However, if the proposed time period to test the new medication is too long, many patients will need symptomatic treatment, and researchers will lose their ability to monitor clinical disease progression. Therefore, most trials of potential disease slowing medications in early PD observe patients for about six months to a year.
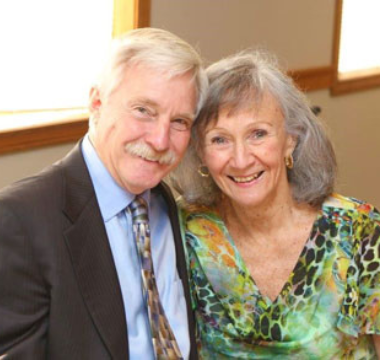
However, if the proposed time period to test the new medication is too long, many patients will need symptomatic treatment, and researchers will lose their ability to monitor clinical disease progression. Therefore, most trials of potential disease slowing medications in early PD observe patients for about six months to a year. This article was written by Robert A. Hauser, MD, MBA, University of South Florida Parkinson's Disease and Movement Disorders Center, a Parkinson’s Foundation Center of Excellence. Dr. Hauser’s primary research interest is in the development of new medical and surgical treatments for Parkinson's, tremor, tardive dyskinesia, dystonia, and restless legs syndrome.
This article was written by Robert A. Hauser, MD, MBA, University of South Florida Parkinson's Disease and Movement Disorders Center, a Parkinson’s Foundation Center of Excellence. Dr. Hauser’s primary research interest is in the development of new medical and surgical treatments for Parkinson's, tremor, tardive dyskinesia, dystonia, and restless legs syndrome.