Hospital Safety Guide
Advocate for your best care with the Hospital Safety Guide.

💡 Quick Summary
-
People with Parkinson’s are at higher risk during hospital stays and should prepare ahead to manage symptoms and prevent complications.
-
The Hospital Safety Guide offers tools like medical alert cards, medication forms and step-by-step planners to support safe hospital visits in the U.S.
-
Planning includes surgery preparation, alternative medication methods, device-specific needs and using smartphone Medical ID for emergencies.
People with Parkinson’s disease (PD) are at a higher risk of hospitalization and face many challenges while in the hospital. It is important for all people with Parkinson’s to be aware of the risks, prepare ahead of time and know how to advocate for their needs while in the hospital.
The Hospital Safety Guide is a resource for people with Parkinson's and their care partners filled with useful tools and information to prepare for and navigate a hospital stay.
The Importance of Hospital Safety
For most people, being in the hospital is a stressful experience. People are usually sick or experiencing some kind of health crisis. For people with PD, symptoms may get worse, and new symptoms, like confusion or thinking changes, can develop because of stress, infection, fatigue, sleep disturbances, surgery or new medications.
Already a delicate balance, PD symptom management can be even trickier in the hospital because:
- People often do not get enough movement opportunities.
- Parkinson’s medications may not be given following the at-home schedule.
- Medications that worsen PD are sometimes prescribed.
- PD medication doses are often delayed or missed.
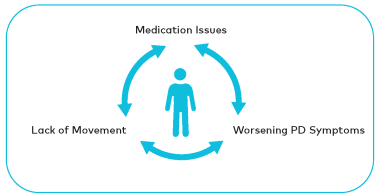
These issues can lead to additional complications and set up a vicious cycle that puts you at risk for falls, swallowing changes, muscle deterioration, medication side effects, mental and physical decline or decreased independence. This is known as “The Symptom Spiral.”
Order your free Hospital Safety Guide
At the Parkinson’s Foundation, it is our mission to help people with Parkinson’s disease live better lives, and that includes staying safe while in the hospital. Our Hospital Safety Guide is available to everyone in the Parkinson’s community at no cost to order or download.
We currently only ship the guide within the U.S. If you are outside the U.S., we recommend downloading the guide and printing the essential resources outlined below.
Guide Resources
The Hospital Safety Guide is filled with useful tools and information to help a person with Parkinson’s during their next hospital visit, planned or unplanned. Print these resources when you have used the copies within your guide, or share additional copies with care partners and loved ones.
Hospital Safety Forms
Medical Alert Card
Fill in your card with emergency contact information and place it in your wallet.
Medication Form
Complete this form every time your medication routine changes. Keep copies with your guide for use at the hospital. If you download the form, you can fill it out on your device before printing.
Parkinson’s Care Summary for Health Professionals
Hospital staff may not be familiar enough with PD to understand your symptoms, know why they fluctuate or that they can worsen quickly if you do not receive your Parkinson’s medications at the scheduled times. Share this summary with health professionals providing your care to ensure they know what you need.
Doctor’s Letter: Parkinson’s Hospital Care Needs
Ask your primary Parkinson’s care provider to sign this letter, which highlights the impact that infections can have on Parkinson’s symptoms and the importance of adherence to the Parkinson’s medication schedule.
Device-Specific Needs
If you have received any surgical treatments for Parkinson’s, fill out this form and keep any device-specific information with your guide.
My Personal Care Details
Use this form to keep track of information that is specific to you and your care.
Print All Forms
Print all forms from the Hospital Safety Guide, outlined above, as a single PDF document.
Additional Important Resources
Your Step-by-Step Hospital Planner
Review this planner before you need it. When it comes to hospital safety, planning is best. You can also use this planner to help get you up-to-speed quickly in case of an emergency!
My 5 Parkinson’s Needs
Refer to these pages while you or your loved one are in the hospital. Each page outlines the importance of a Parkinson’s need, real-time steps to have each need met, common challenges and important things to understand.
Preparing for Surgeries and Other Procedures
Review these recommendations before surgery and refer to them on surgery day.
Other Ways to Take Your Medication
Review these options if you are told that food, water and/or medication must be withheld prior to a surgery or other procedure, or because of concerns with swallowing ability.
Using Medical ID on your Smartphone
Medical ID is a tool on Apple and Android smartphones that is used by first responders if you are unable to communicate and have your phone with you.
Interested in having a Parkinson’s Foundation Ambassador speak to your group?
Parkinson’s Foundation Ambassadors are trained volunteers who talk to clinicians, healthcare professionals, support groups and many others about the Hospital Safety Guide and hospital care for people with PD. If you are interested in inviting an ambassador to speak to your group, in person or virtually, please fill out a Parkinson’s Foundation Ambassador Engagement Request. If you are interested in sharing important hospital care information and becoming a Parkinson’s Foundation Ambassador yourself, visit Parkinson.org/Volunteer.

"My passion has become educating people with Parkinson’s and their families about how they can live a great life despite their PD diagnosis. I wanted to share how the Hospital Safety Guide could be a useful tool in achieving that.”
Join the Fight Against Parkinson's
Support ground-breaking research, care and community outreach