My PD Story

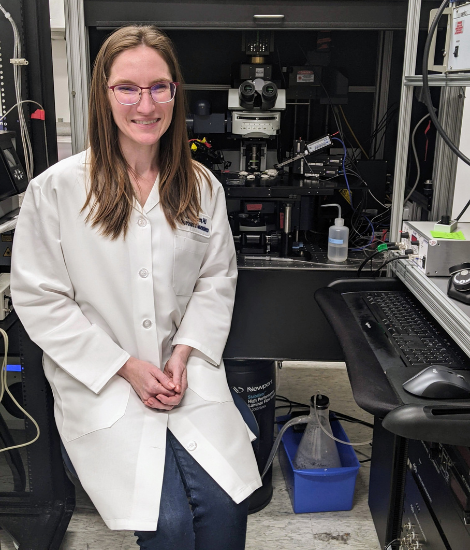
Kaitlin Lansford, PhD
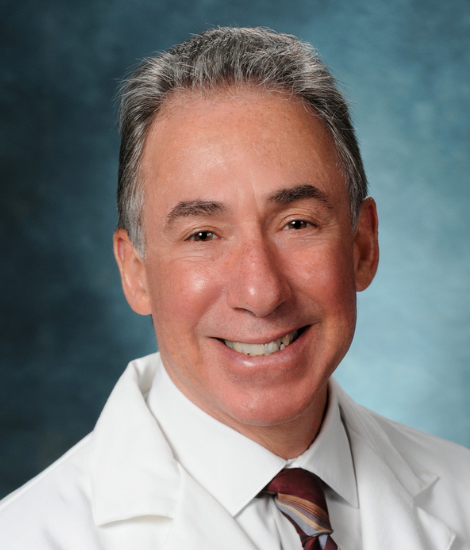
2023 Impact Award
Overcoming Communication Barriers and Improving Well-being with Listener Training
Most people know about the movement symptoms of Parkinson’s disease (PD), but they do not usually think about how the disease impacts communication. Research shows that up to 90% of people with PD may develop hypokinetic dysarthria, a disorder that affects a person’s physical speaking ability. This disorder contributes to decreased intelligibility of those affected, greatly impacting their ability to communicate with others. Common interventions focus solely on the patient (speaker) to improve their speech. Kaitlin Lansford, PhD, recipient of a Parkinson’s Foundation 2023 Bill and Amy Gurley Impact Award, seeks to improve the social well-being of those with PD experiencing this speech disorder by investigating whether listening training for their care partners can help overcome these communication barriers.
The two main speech consequences of hypokinetic dysarthria are reduced volume and imprecise articulation. Therefore, speech therapy for those with hypokinetic dysarthria is often focused on having the person speak louder and more clearly. Such speaker-targeted interventions can improve intelligibility, but its effectiveness is limited, especially when related physical and cognitive symptoms are more severe. Dr. Lansford, director of the Motor Speech Disorders lab at Florida State University, in collaboration with her research partner, Dr. Stephanie Borrie from Utah State University, has demonstrated that listeners can be trained to better understand dysarthric speech. Such listener-based interventions have the potential to improve communication without increasing the communicative burden of the person with PD. With care partners often wanting to have a more active role in the rehabilitation of their loved ones, listening training has great potential for improving the social lives of those with PD.
To better understand how listening training can be used to complement commonly used speaker interventions for those with PD-associated hypokinetic dysarthria, Dr. Lansford will conduct a study in which 20 speakers with PD and hypokinetic dysarthria and 600 listeners will be recruited to participate in a series of speaking and sensory tasks. The speakers will provide speech samples and will be cued to speak, louder, more clearly or in their normal speaking voice. The speech samples will be used to generate perceptual experiments. The recruited listeners will be randomly assigned to one of the speaker training conditions and half (300) will engage in listening training, in which they will benefit from a familiarization experience with feedback. The other half of listeners (300) will not receive listening training. All listeners will transcribe the speech samples and these transcriptions across the different speaker and listener training conditions will be scored for intelligibility, after which the impact of combined training can be properly assessed.
“Receiving the Parkinson's Foundation Impact Award to support this research project is a true honor,” said Dr. Lansford. “Given that most daily communication for people over 65 years occurs with family and friends, a dual [speaker and listener] treatment approach has the potential to significantly and positively impact the lives of people with PD and their key communication partners. [This award] will greatly enhance the visibility and impact of our findings, opening doors to future collaborations, grants, and opportunities to support this line of research, thereby advancing therapeutic interventions and enhancing patient care in PD.”
Meet more Parkinson’s researchers! Explore our My PD Stories featuring PD researchers.
Related Materials
More Stories
from the Parkinson's community