Marijuana and Parkinson's: What Do We Really Know?

People with Parkinson’s disease (PD) and their physicians are both looking to answer whether medical marijuana can help manage Parkinson’s symptoms. Researchers have barely scratched the surface when it comes to marijuana and PD and previous studies are inconclusive about its potential benefits, but many people with Parkinson’s are curious to try it. Here’s what you need to know.
The following article is based on the latest research and a Parkinson’s Foundation Expert Briefings about marijuana and Parkinson’s hosted by Benzi M. Kluger, MD, MS, Associate Professor at Neurology and Psychiatry at University of Colorado.
What’s in Marijuana?
Marijuana itself — the dried leaves known by names like pot and weed — comes from a genus of flowering plants called Cannabis. Cannabis plants contain more than 100 chemicals, called cannabinoids, which affect the human nervous system. Some of these chemicals stimulate parts of the brain, while others block the same effects.
The best-known plant-based cannabinoids are:
- THC (D9-tetrahydrocannabinol): the psychoactive component of Cannabis responsible for making a person feel “high.” Sativa strains of Cannabis (Cannabis sativa) tend to have higher THC concentrations than others. Marijuana available today typically has 10 to 30 times the amount of THC as that from the 1970s.
- CBD (cannabidiol): the component of cannabis that may have calming effects on the nervous system. It does not have the psychoactive effects of THC. The indica and rudaralis strains of Cannabis (Cannabis indica and Cannabis rudaralis) tend to have less THC and more CBD.
Marijuana Research
Endorphins are the naturally occurring substances in the brain that help reduce pain. They are boosted by exercise. Sometimes they are called the brain’s natural opiates, because opioid drugs bind to the same cell receptors as endorphins. Similarly, the brain has its own naturally occurring cannabinoids. Cannabinoids in marijuana have an effect by binding to the receptors for these natural molecules.
The chemicals in the brain that are similar to the active agents in marijuana are called endocannabinoids. Of these, scientists have studied anandamide, which may play a role in pain, sleep and other behaviors, along with the development of the nervous system. The name anandamide means “bliss.” This chemical is found in the human brain and, not surprisingly, in chocolate.
Do endocannabinoids have a role in Parkinson’s? Researchers know that they are involved in the brain area called the basal ganglia, which is affected by PD. Through research, scientists are gaining an understanding of the two main receptors in the brain that respond to marijuana:
- CB1 (primarily in the central nervous system)
- CB2 (primarily in the immune system).
The dozens of different cannabinoids in marijuana have a range of effects to activate or block receptors.
In studies with laboratory animals, cannabinoids that bind to CB1 have been reported to improve dyskinesias, the involuntary movements that can develop after several years of taking levodopa therapy. Cannabinoids also have antioxidant and anti-inflammatory effects, which could point to neuroprotective activity. Some studies support this idea, but more research is needed.
Cannabinoids synthesized in the laboratory (rather than extracted from marijuana) have been tested as therapies for diseases other than Parkinson’s. CBD recently was approved as a therapy for rare types of epilepsy. Two synthetic cannabinoids are sold as FDA-approved therapies for nausea and other side effects of cancer chemotherapy:
- Marinol (dronabiol): synthetic THC
- Nabilone: a cannabinoid that acts on both CB1 and CB2
Warning: Synthetic Marijuana
Synthetic marijuana, sold legally under names such as K2 and Spice, contains lab-made cannabinoids and other chemicals. Synthetic marijuana can cause severe, even deadly, side effects. It is not a substitute for plant-based marijuana and remains unregulated.
Clinical Studies
Few studies have enrolled people with PD to investigate the effects of cannabinoids on Parkinson’s symptoms. So far, the most rigorous clinical studies of cannabis and PD movement symptoms have been inconclusive at best, because of the small numbers of participants and other limitations.
In other, less rigorous studies, researchers have surveyed cannabis use among people with Parkinson’s. In these surveys people reported their own experiences, without comparison to a control group. Small numbers of participants reported that cannabis helped tremor, slowness, and non-motor symptoms such as pain, sleep difficulties, anxiety and loss of appetite.
Research is under way to better understand how specific cannabinoids might affect PD symptoms, including a study of the safety and effectiveness of CBD for tremor. In addition, research suggests that CBD could be calming for people with Lewy body dementia, a disease related to Parkinson’s. Research shows that people with dementia should avoid marijuana or other products that contain THC.
Side Effects
With the help of the internet, marijuana and Parkinson’s remains a hot topic. In an era where certain self-help books promote marijuana for Parkinson’s, it’s important to keep in mind that cannabis is not a performance-enhancing substance.
Keeping in mind the comedic duo from the 1970s, Cheech and Chong, marijuana makes people move slowly. Other common side effects include:
- Cognitive slowness
- Worsening apathy, lack of motivation
- Memory problems
- Low blood pressure, leading to dizziness and an increased risk of falls
- Increased lung cancer risk or other pulmonary issues from smoking
- Experiencing uneasiness and feeling unwell due to edible cannabis products, which may have less predictable absorption into the body and different dosages
Guidelines for Medical Marijuana and Parkinson’s
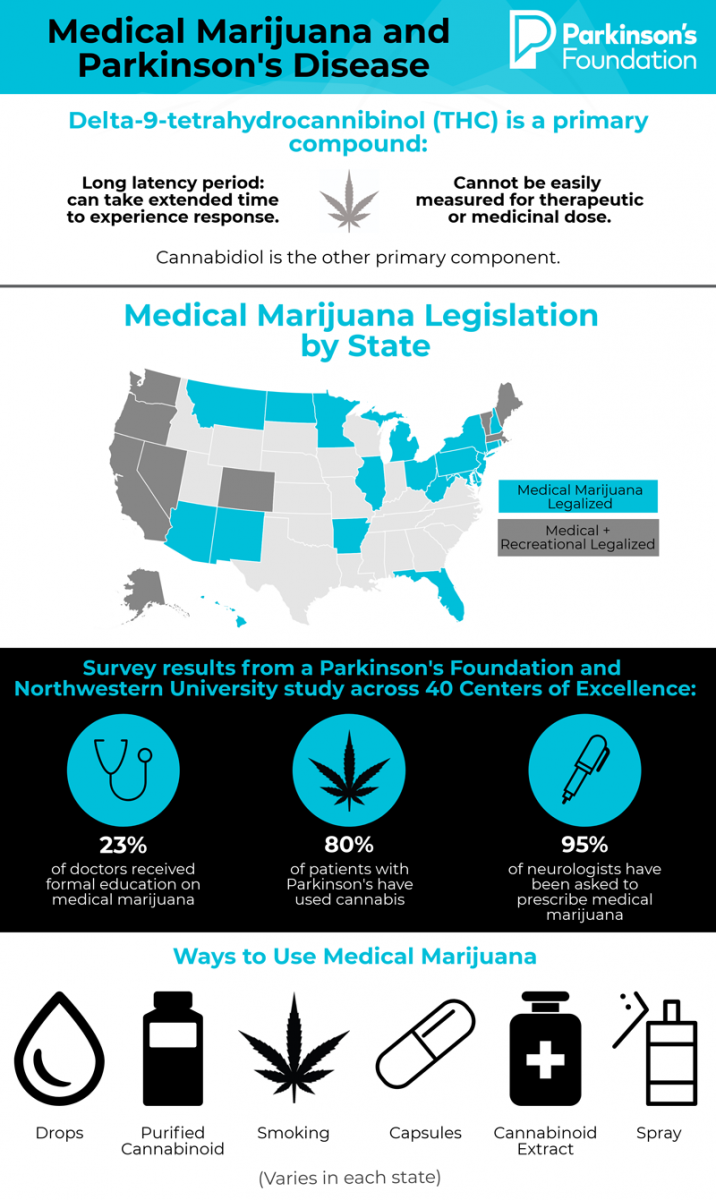
Medical marijuana is legal in 29 states, as of early 2018. If you decide to try it for your PD symptoms:
- Inform your doctor. Both you and your doctor should be aware of potential interactions with other drugs, including entacapone (Comtan®) and citalopram (Celexa). Some physicians are not receptive to the use of medical marijuana or are not comfortable filling out state-mandated paperwork. If that’s the case, consider finding a physician who will work with you. Medical marijuana should be approached as a complementary therapy and never a substitute to medication.
- Be aware that cannabis products are not regulated. There is no assurance that one product that says it contains 10 mg of CBD is the same as another.
- Not all marijuana products are the same. Even if two products are the same strain, for example, the cannabinoids in them may be different, and have different effects.
- Stay consistent. To get the most consistent dose, stay with the same product, obtained from the same dispensary or source.
- Start with a low dose. As with all medications, start with a low dose and observe the effects. If you increase the dose, do it gradually.
- Avoid smoking. Oral drops are an alternative.
- Try skin creams or patches for localized pain. Use it like an analgesic cream for certain areas, like the legs.
Conclusion
Cannabis, the marijuana plant, contains more than a hundred different psychoactive chemicals, which have complex effects. Products derived from cannabis may vary widely in terms of their benefits and side effects.
There is currently no conclusive scientific research supporting the benefits of cannabis for any aspect of Parkinson’s. However, anecdotal evidence suggests that cannabis may help pain, sleep, appetite, nausea and anxiety. People with Parkinson’s should especially be aware of side effects such as confusion and low blood pressure that may exacerbate PD symptoms.
For more insights on this topic, listen to our podcast episode “A Western Perspective on PD: Understanding Complementary Medicine”.
Related Blog Posts

Mapping the Brain in High Resolution: How the University of Michigan is Advancing Parkinson’s Neuroscience

Neuro Talk: Newly Diagnosed
