Planning Ahead

There are a lot of day-to-day tasks and responsibilities that are necessary to help you care for your loved one with Parkinson’s disease (PD), but it is never too soon to begin planning for the future.
It is okay if you feel like you need to get a handle on the present before the future, but it is important to have these discussions sooner rather than later. Planning can seem extremely overwhelming, so we broke it down into sections for you:
Logistical Planning
Caring for someone with Parkinson’s means keeping track of medical records, medical and family contact lists, financial documents and other critical information. Below are some tips on what information to gather and how to keep it all organized.
Getting Organized
Consider creating a binder with the following main document categories:
- Medical
- Family
- Insurance/Property
- Finance
Even though you can now keep digital files, it can be useful to have a physical copy of key documents in one place. Wherever you choose to maintain your records, make sure that a close family member or friend knows where to find them in case of emergency.
Remember, it’s not all about the person with Parkinson’s. Make sure to keep your records organized, too!
Emotional Planning
You will experience a range of emotions over the course of your loved one’s Parkinson’s journey. Shock and denial at diagnosis, or validation that your suspicions were confirmed; fear of the loss of control; frustration as symptoms worsen; satisfaction from caring for a loved one; concern about finances; shame because you wish it were all over; exasperation, relief, anger, sadness, joy. As the disease progresses and your role as caregiver evolves, you will have to come to terms with the disease again and again.
Caregiving is a demanding job. There is always something else that could be done, so feelings of guilt that you cannot do everything are normal. Ask yourself if doing more is necessary or possible. Accept your limits.
As Parkinson’s progresses, it is hard to let go of the hope that your loved one might return to his or her former self or that things will go back to “normal.” Even when you have the diagnosis, know the facts and witness the effects of the disease, you might still feel like your relative could be the one who beats the odds.
In addition, family dynamics add complexity, and past feelings can affect how you respond to situations now. The historical relationship between care partners has a huge impact on how care is given and decisions are made. Real-life examples illustrate this point:
Ultimately, caring for yourself mentally and emotionally requires understanding the changes in the person you’re caring for and adapting to them. The relative or friend you’ve always admired for his strength might be showing weakness; on the other hand, his perseverance and optimism in the face of debilitating illness might demonstrate strength you never knew he had. Your emotions throughout the journey will be varied, and some might surprise you.
It is important to be honest with yourself about what you feel and to have an outlet for your emotions. Some of these emotions will be appropriate to share with your loved one, but some will not. Make sure you have a person or group you are comfortable sharing your feelings with, so you can freely express everything that is on your mind.
Join a Support Group
If you need help locating a support group, contact the Parkinson’s Foundation Helpline at 1-800-4PD-INFO (1-800-473-4636) or helpline@parkinson.org.
Palliative Care
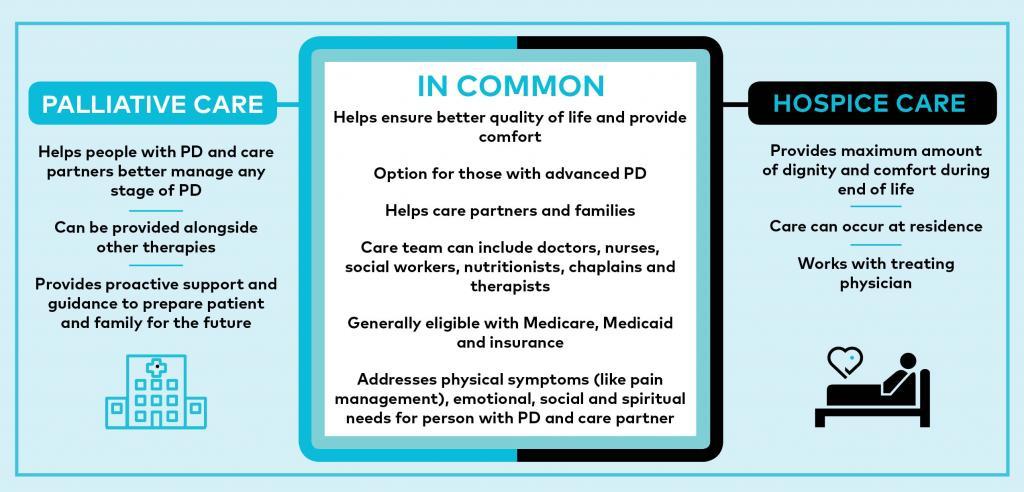
Just as a healthy diet and ample exercise can help you live optimally with Parkinson’s, so can palliative care. Palliative care — sometimes mistaken for end-of-life, or hospice, care — is instead holistic, team-based treatment designed to support a person’s quality of life from the point of their diagnosis onward.
Studies have shown that people who receive palliative care experience:
- Less pain and other adverse symptoms like nausea or shortness of breath
- Better communication with their doctors and family members and experience more emotional support
- Receiving care is more in line with their wishes and meets their emotional and spiritual needs
Palliative care is usually provided by a team of professionals that may include doctors, nurses, social workers, chaplains, pharmacists, nutritionists, counselors and others. Most insurance plans cover all or part of the palliative care treatment costs. If the person with PD is an enrolled veteran, palliative and hospice care are part of the Standard Medical Benefits Package if the need for clinical service requirement is met.
If you are worried about the cost of this type of treatment, the social worker from the palliative care team can help answer your questions. The palliative care team can help people with PD and family members make decisions about treatment options in advanced disease and can segue into hospice care if that is desired.
One major benefit of palliative care is the emphasis on taking the time to understand your treatment preferences and goals. This process puts more control into you and your loved one with Parkinson’s hands.
Advance Care Planning
Advance care planning is a valuable process for you and your loved one to align your values, wishes and preferences with medical care you wish to receive.
When starting the conversation, discuss a situation where your loved one would be unable to make their own medical decisions. Advance care planning is recommended for all adults, in all stages of health.
When to Plan
It is never too early to plan. It is ideal to initiate an advance care planning discussion when your loved one with Parkinson’s can fully participate and share their wishes regarding what types of medical care they want to receive in the event of life-threatening symptoms.
The Conversation Project can help you and your loved one think about and begin to discuss your wishes for end-of-life care.
Advanced Parkinson’s
When a person with PD has problems with mobility and cannot complete activities of daily living without help, this is generally known as advanced Parkinson’s. Explore our articles and tips created to help care partners navigate this next stage.

Who should be involved?
Frank, open discussions can be difficult. Not all people are comfortable talking about this delicate subject with others. Although it is not always easy, many people report a sense of relief and optimism sharing their thoughts and wishes.
It can be helpful to include a social worker, chaplain or other medical team representative with experience in advance care planning in your family’s discussion. These professionals can also help create the necessary documents and assist with obtaining the necessary signatures and authorizations required to create a legal document.
Sometimes people work with a lawyer to finalize these documents, but this should be the final step, not the first step, because it is essential that you, your love one, and their healthcare team all understand your loved one’s preferences.
Read our Legal, Financial & Insurance Articles
How to Start the Process
One way to jump-start the process is to look at the Advanced Directive forms in your state. Consider printing the form and bringing it to your next medical appointment. Ask your doctor to talk to you about their advance care planning process or ask them to help you find a social worker to discuss it with.
Visit the AARP Advanced Directive Forms page to find the form used in your state.
Related Materials
My Parent Has Parkinson's. What Does It Mean?
Intimacy and PD
Impulse Control
Related Blog Posts


Top 10 Essential Caregiver Resources
